Background and Objectives: In 2018, the 25 x 2030 Collaborative was created. Its goal is to “increase the proportion of US medical school graduates who choose family medicine (FM) to 25% by 2030.” The purpose of this study was to take a deeper look at the history of medical student interest in FM from the earliest data to the present, both after the match and those who are FM interns after July 1.
Methods: We used publicly available match data, primarily from the National Resident Matching Program website, a series of articles published for nearly 30 years in Family Medicine on match results, and the American Academy of Family Physicians website.
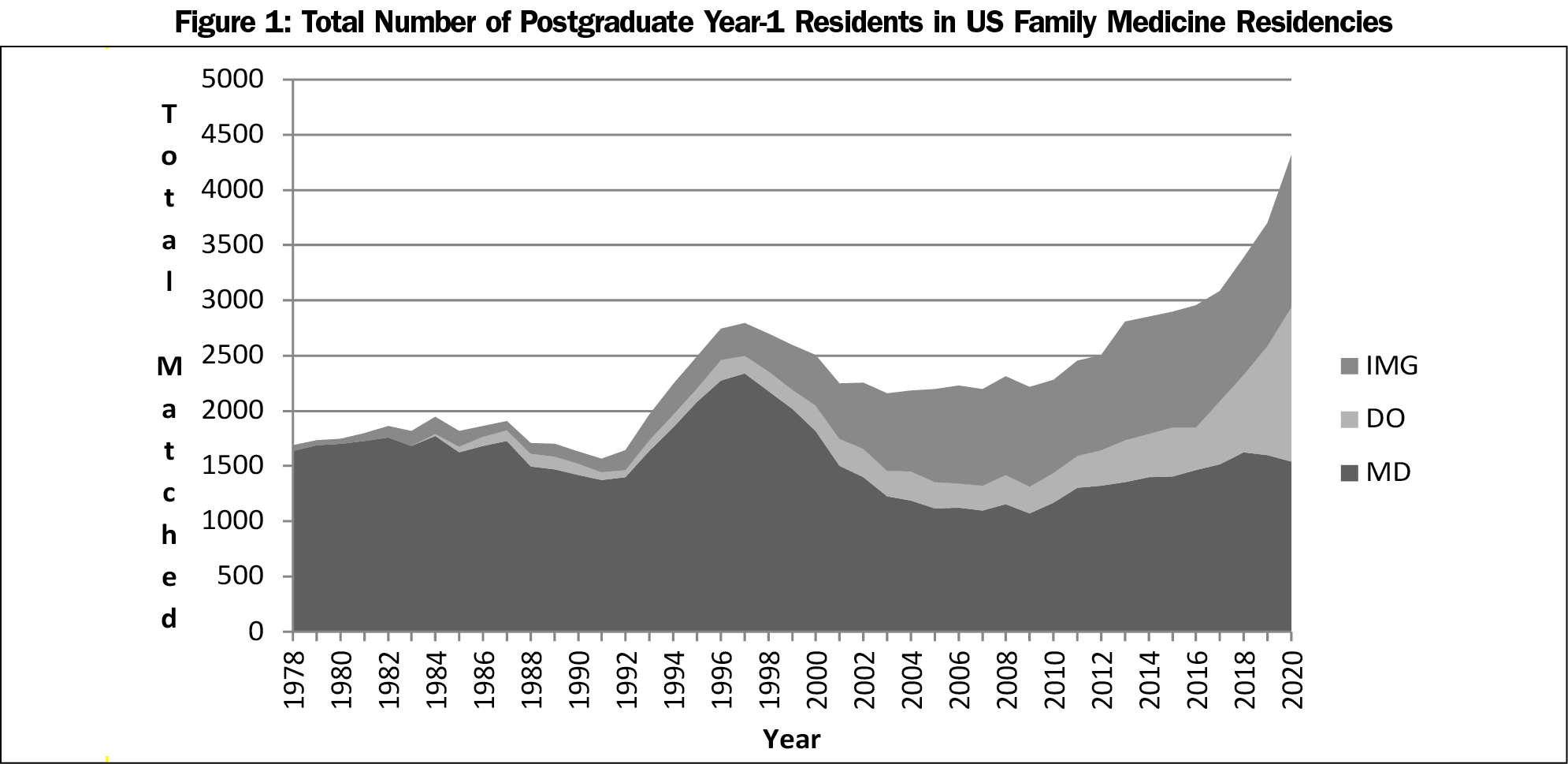
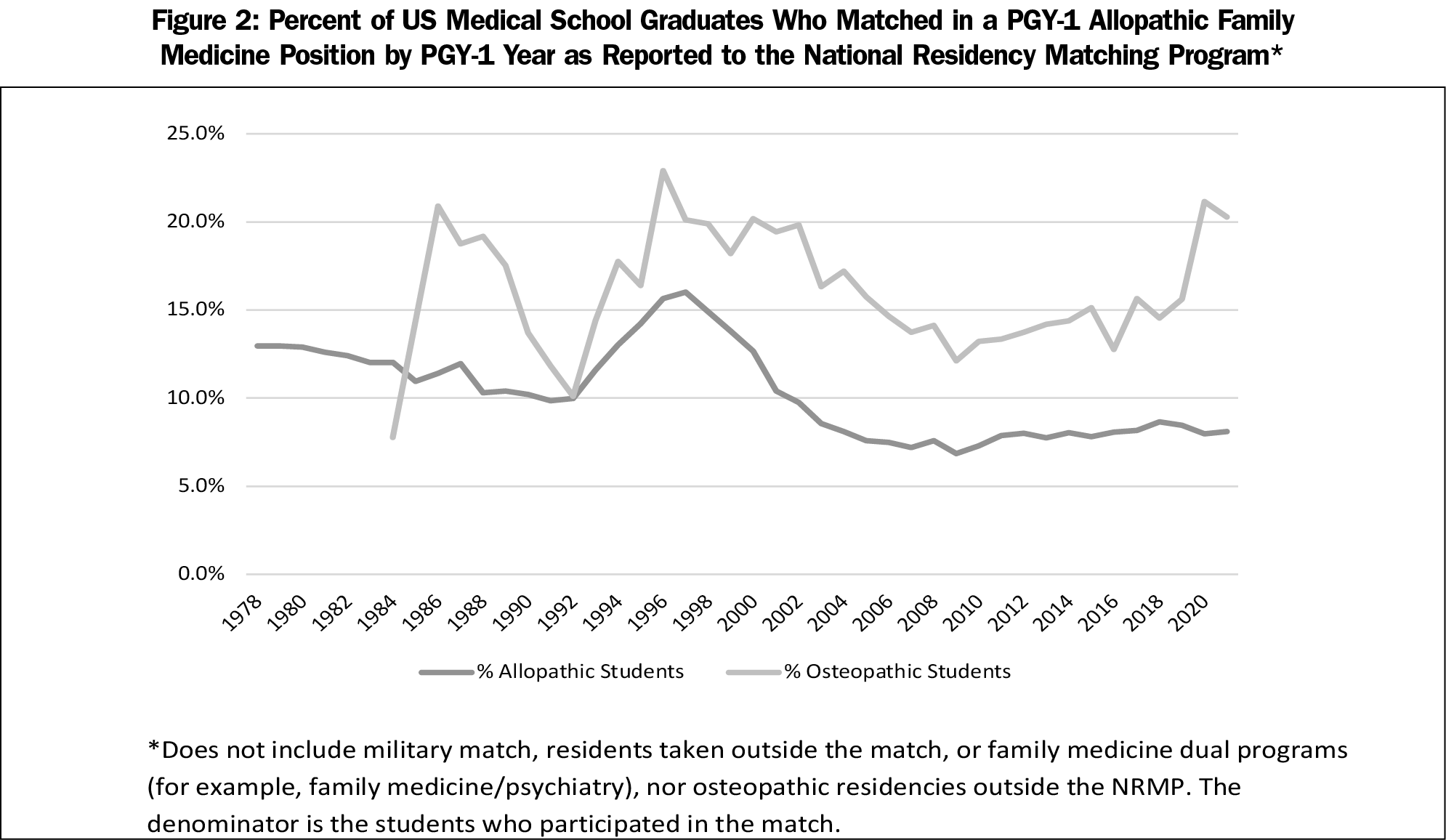
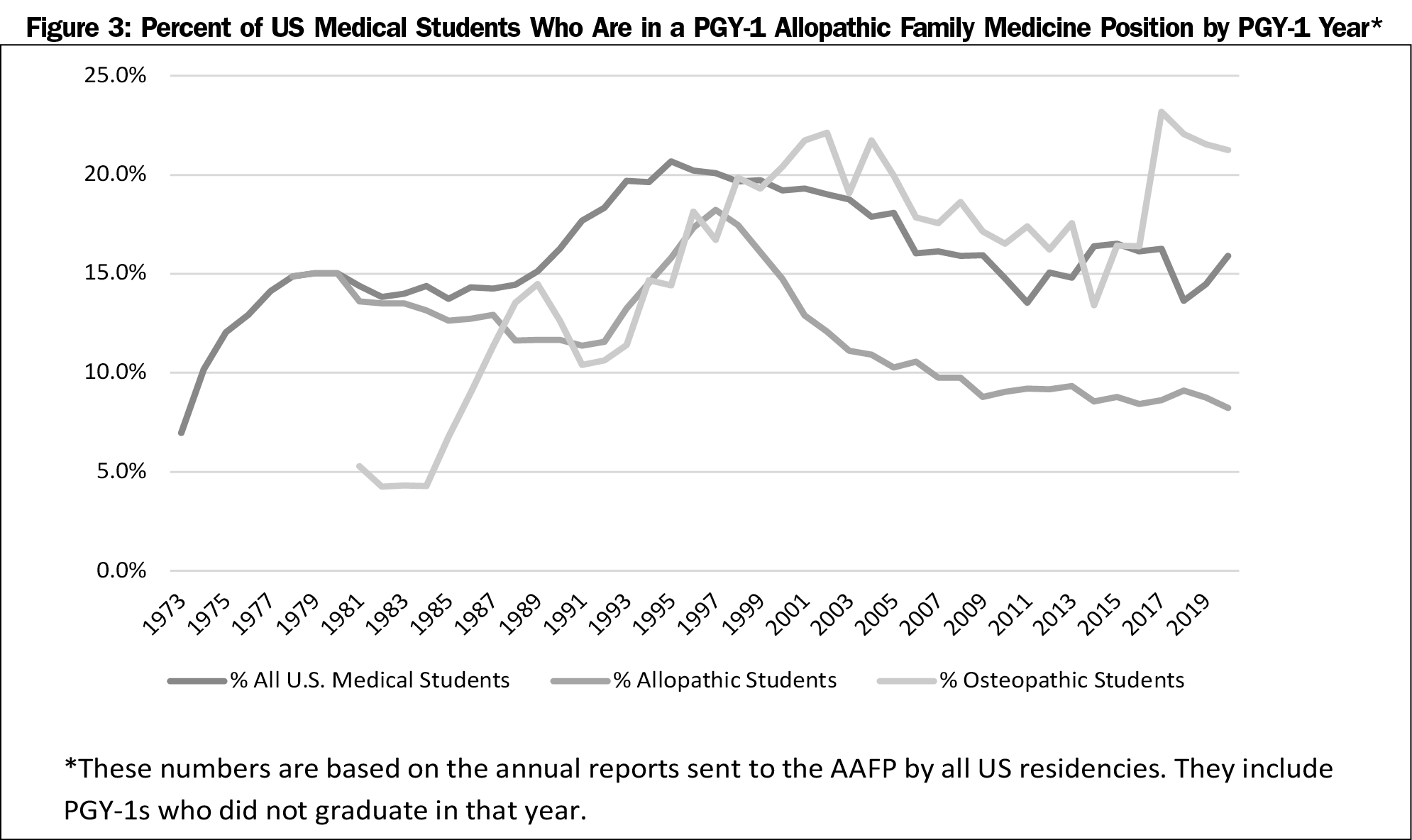
Results: The total number of FM residents is growing (4,493 matched in 2021). After the managed care era in the mid-1990s, there was a collapse in interest among allopathic graduates that bottomed out at 6.8% graduates matching in FM by 2009; this rate has only slowly increased to 8.1% in 2021. Interest has been essentially flat for the last 10 years, and is lower than the percentage match rate prior to the managed care era (9.9% to 14.0%). There was more variability among osteopathic students, but interest has never been greater than 23%. Including the allopathic and osteopathic students who join FM residencies after the match does not appreciably alter these results.
Conclusions: The 25 x 30 Collaborative will likely fail to reach its goal.
In 2018, eight family medicine (FM) organizations collaborated to launch the 25 x 2030 Collaborative.1 It was created for many reasons, including the predicted worsening of the primary care physician supply,2 and the positive effects of primary care supply on population health outcomes and total costs of care.3-6 The goal of 25 x 30 is to “increase the proportion of US medical school graduates who choose to go into family medicine to 25% by 2030.”1
The 25 x 30 goal represents a huge challenge. In 2021, only 8.1% of US allopathic senior medical students matched in FM, 22.8% of osteopathic students, and 12.6% of US medical students or graduates overall.7 A review of recent match results found the prospects for success of the 25 x 30 goal are not good.8 The purpose of this study was to take a deeper look at the history of medical student interest in FM from the earliest data to the present.
We used publicly available match data, primarily from the National Resident Matching Program (NRMP) website,9 a series of articles published for nearly 30 years in Family Medicine on match results (examples10, 11), and the American Academy of Family Physicians (AAFP) website.7 We calculated the percentage of medical students who choose FM in two ways. One was based only on the NRMP data of the match. We chose to include the types of residencies in the numerator to be consistent with past reports of the NRMP and AAFP.
The second way was based on FM residencies’ reports to the AAFP of the intern classes after July 1. This number reflects the interns who were accepted outside the match (the Supplemental Offer and Acceptance Program [the “scramble”] and other contracts offered outside the match). This figure includes students who graduated in years prior to the index year (they did an internship in another specialty, then switched to FM).
We used descriptive statistics to analyze the data. This study used publicly available data and was classified as non-human subjects research.
The total number of people who entered FM residencies as interns, by year, is shown in Figure 1.
The percentages of US allopathic and osteopathic senior medical students who matched into FM residencies through the NRMP is shown by year in Figure 2. After the managed care era in the mid-1990s, there was a collapse in interest among allopathic graduates that bottomed out at 6.8% for FM by 2009 and has only slowly increased to 8.1% in 2021. This percentage has been essentially flat for the last 10 years. This is lower than the percentage match rate prior to the managed care era of 9.9% to 14.0%.
Figure 3 shows the percentage of students who were present as interns in FM residencies on July 1 (with the denominator of all medical school graduates that year).
There is a wide gulf between the number of US medical students who match into FM and the 25% goal of the 25 x 30 initiative. This is true for both allopathic and osteopathic medical students. This gulf has shown little sign of shrinking since the 25 x 30 initiative was announced. Even including FM interns who were not accepted in the match does not alter this conclusion.
The recent large increase in osteopathic student numbers is mostly explained by the transition of osteopathic residencies to common accreditation standards and inclusion in the NRMP from 2015 to 2020 (There is no longer a separate osteopathic residency match). This explains why the rapid increase in FM intern total numbers does not translate into a higher percentage of student interest, which is the goal of 25 x 30.
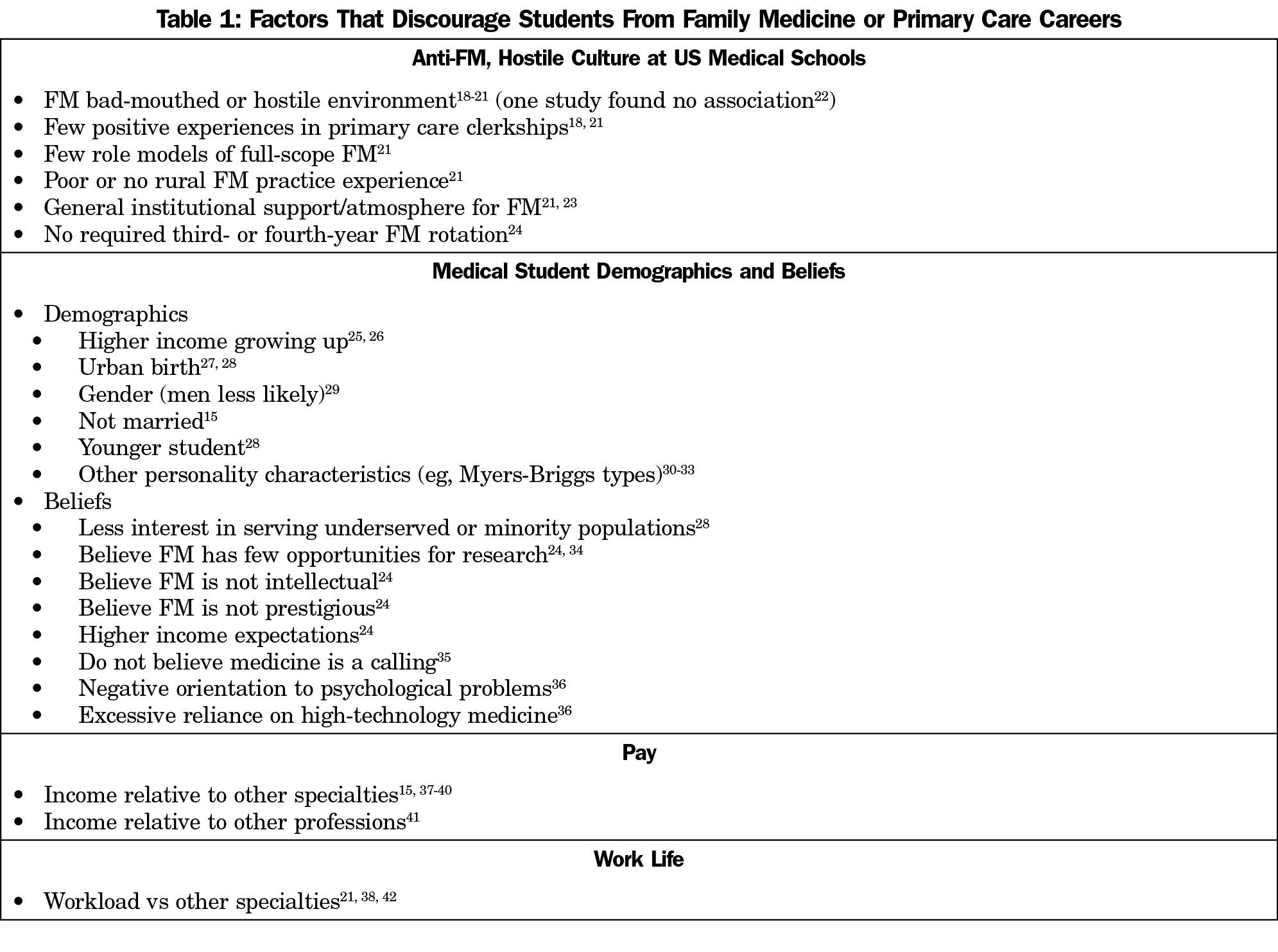
There are many reasons medical students choose not to pursue careers in family medicine. Table 1 summarizes the literature in this area. In contrast to a common belief, medical student debt has little influence on family medicine or primary care career choice.12-14 In contrast, the Robert Graham Center report on predictive factors stated, “[t]he income gap between primary care and subspecialists has an impressively negative impact on choice of primary care specialties and of practicing in rural or underserved settings.”15
One of the limitations of this study is that previous reports on medical student interest in family medicine were inconsistent. For example, in the 2005 match, the number was reported in different publications as 2,761,9 2,782,16 and 3,522.17 This discrepancy was explained by differences in reporting the results of the NRMP (“the Match”), which residencies were included (military and osteopathic were not included in the NRMP reports, and reports were inconsistent in how they handled dual programs, FM-Psych for example), and which students became interns in July.
Also of note, we could find no studies investigating the impact on medical students’ career choice of electronic medical record use or burnout observed in physicians.
After the managed care era, none of the primary care-centered reforms from the early 2000s to the present have significantly moved the needle on medical student interest in family medicine. There are no indications in the present environment (reimbursement by specialty; legislative mandates, new strategies to increase student interest in family medicine, the COVID-19 pandemic, or anything else) to suggest that the current trends will change over the next 9 years. The 25 x 30 initiative may even have created an unintended negative consequence by contributing to the demoralization of family physicians by bringing attention to the continued lack of student interest in FM or primary care.
The 25 x 30 Collaborative will almost certainly fail to reach its goal. Bolder reforms in the US medical school culture, and the income and daily work life of family physicians will be required to achieve the goal of 25% of US medical students choosing FM.
Acknowledgments
The authors thank Ashley Bentley, MBA, of the AAFP for helping us understand details of previous match data reports, and Sam Grammer, of the Society of Teachers of Family Medicine for helping us access archived copies of Family Medicine.
Presentations: A preliminary version of this study was presented a JPS Research Day, in Fort Worth, Texas, in June 2021.
Conflict Disclosure: Dr Young discloses that he is the sole owner of SENTIRE, LLC, a primary care documentation, coding, and billing system. Dr Tinger has no conflicts to disclose.
References
- Prunuske J. America Needs More Family Doctors: The 25 x 2030 Collaborative aims to get more medical students into family medicine. Am Fam Physician. 2020;101(2):82-83.
- Wilkinson E, Bazemore E, Jabbarpour Y. Ensuring primary care access in states with an aging family physician workforce. Am Fam Physician. 2019;99(12):743.
- Basu S, Berkowitz SA, Phillips RL, Bitton A, Landon BE, Phillips RS. Association of primary care physician supply with population mortality in the United States, 2005-2015. JAMA Intern Med. 2019;179(4):506-514. doi:10.1001/jamainternmed.2018.7624
- Phillips RL, Dodoo MS, Green LA, et al. Usual source of care: an important source of variation in health care spending. Health Aff (Millwood). Mar-Apr 2009;28(2):567-77. [pii] doi:10.1377/hlthaff.28.2.567
- Bazemore A, Petterson S, Peterson LE, Phillips RL Jr. More comprehensive care among family physicians is associated with lower costs and fewer hospitalizations. Ann Fam Med. 2015;13(3):206-213. doi:10.1370/afm.1787
- Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457-502. doi:10.1111/j.1468-0009.2005.00409.x
- American Academy of Family Physicians. 2021 Match Results for Family Medicine. 2021. Accessed March 22, 2021. https://www.aafp.org/students-residents/residency-program-directors/national-resident-matching-program-results.html
- David AK. Matching 25% of medical students in family medicine by 2030: realistic or beyond our reach? Fam Med. 2021;53(4):252-255. doi:10.22454/FamMed.2021.982403
- National Resident Matching Program. Main Residency Match Data and Reports. Accessed March 11, 2021. https://www.nrmp.org/main-residency-match-data/
- Pugno PA, McGaha AL, Schmittling GT, DeVilbiss Bieck AD, Crosley PW, Ostergaard DJ. Results of the 2010 national resident matching program: family medicine. Fam Med. 2010;42(8):552-561.
- Kozakowski SM, Travis A, Marcinek JP, Bentley A, Fetter GT Jr. Entry of medical school graduates into family medicine residencies: 2016-2017. Fam Med. 2017;49(9):686-692.
- Phillips JP, Morgan ZJ, Bazemore AW, Peterson LE. Debt of family medicine residents continues to grow. J Am Board Fam Med. 2021;34(3):663-664. doi:10.3122/jabfm.2021.03.200567
- Phillips JP, Peterson LE, Fang B, Kovar-Gough I, Phillips RL Jr. Debt and the emerging physician workforce: the relationship between educational debt and family medicine residents’ practice and fellowship intentions. Acad Med. 2019;94(2):267-273. doi:10.1097/ACM.0000000000002468
- Phillips JP, Petterson SM, Bazemore AW, Phillips RL. A retrospective analysis of the relationship between medical student debt and primary care practice in the United States. Ann Fam Med. 2014;12(6):542-549. doi:10.1370/afm.1697
- Phillips RL, Dodoo M, Petterson SM, et al. What Influences Medical Student & Resident Choices? Robert Graham Center.2009(Mar 2). May 18, 2009. Accessed May 18, 2009. http://www.josiahmacyfoundation.org/documents/pub_grahamcenterstudy.pdf
- Pugno PA, Schmittling GT, Fetter GT Jr, Kahn NB Jr. Results of the 2005 national resident matching program: family medicine. Fam Med. 2005;37(8):555-564.
- Pugno PA, Schmittling GT, Kahn NB Jr; American Academy of Family Physicians. Entry of US medical school graduates into family medicine residencies: 2004-2005 and 3-year summary. Fam Med. 2005;37(8):546-554.



There are no comments for this article.