Background and Objectives: Family physicians routinely manage uncertainty in their clinical practice. During their first year of clinical rotations, medical students learn communication and patient care skills that will influence the care they provide as future physicians. However, little is known about how their reactions to uncertainty change during this formative year, and medical education often fails to teach students how to manage uncertainty effectively. This study employs a repeated measures analysis of students’ reactions to uncertainty over the course of their third year.
Methods: We surveyed 273 medical students at four time points during their third year and employed hierarchical linear modeling to analyze a series of models in which phase and intolerance of uncertainty were entered as covariates. We modeled age and gender as control variables.
Results: Analyses revealed that students’ affective reactions to uncertainty did not significantly change during the third year, but reluctance to disclose uncertainty to physicians and patients significantly decreased across phases. Analyses also showed that general intolerance of uncertainty predicted affective reactions to medical-specific uncertainty.
Conclusions: These findings confirm that students experience negative reactions to uncertainty during clinical rotations. Students would benefit from curriculum designed to mitigate consequences of negative affective reactions to uncertainty, particularly those students characteristically higher in intolerance of uncertainty. Given that students demonstrated more willingness to communicate about their uncertainty over time, medical school should equip students with the communication skills needed to discuss their uncertainty effectively with patients and preceptors.
Given their broad scope of practice, family physicians often report more uncertainty than physicians in non-primary care specialties.1 Unfortunately, physicians often experience anxiety from uncertainty,2 and the culture of medicine often encourages physicians to suppress uncertainty in an attempt to maintain trust and credibility.3 These reactions to uncertainty are shaped early in medical training. Medical students experience high uncertainty due to their limited medical knowledge.4 When faced with uncertainty, students may be insecure of their skills and afraid of making mistakes.5 Consequently, students may fail to express uncertainty in clinical situations.6,7
Students with a lower tolerance of uncertainty are more likely to develop negative attitudes toward underserved populations, experience psychological distress and burnout, and demonstrate decreased capacity for leadership.8–11 Later in their career, suppressing uncertainty can lead to diagnostic errors, excessive tests, unnecessary treatment, increased hospitalizations and referrals, and decreased patient satisfaction.12,13 Therefore, it is vital to address reactions to uncertainty early in a physician’s career. In fact, recent graduates have called for more training during undergraduate medical education to prepare them to manage the uncertainty they will confront in clinical practice.14 Clinical education may be an ideal time to address uncertainty.15 During their first year of clinical rotations, students encounter new clinical scenarios and establish communication skills that will influence the care they provide as future physicians. Previous research has examined students’ intolerance of uncertainty during training.16,17 However, more research is needed to understand students’ affective and behavioral reactions to uncertainty during clinical encounters. Specifically, this study aimed to understand how students’ reactions to uncertainty change during rotations (RQ1), which is necessary to develop effective curricular interventions.10
Moreover, there is debate about whether students’ tolerance of uncertainty is a state or trait characteristic.18,19 Both trait and state approaches to studying uncertainty are important. Trait-focused approaches help identify individual-level differences, whereas state-focused approaches reveal environmental factors that affect students’ reactions.18 Students’ reactions during rotations are likely a result of both individual and environmental factors. Therefore, we hypothesize that intolerance of uncertainty positively predicts reactions to uncertainty (H1).
Author A.M.K.’s institutional review board approved the study (#18-E-252). We invited third-year students beginning clinical rotations to complete an online survey at third-year orientation and every 12 weeks thereafter. We tracked responses using participant-generated identification numbers. Despite some intermittent attrition, sample characteristics at each phase represented the characteristics of the student body at the school (Table 1). Students received Amazon.com gift cards for completing each survey.
Instrument
We measured students’ baseline intolerance of uncertainty using the 12-item Intolerance of Uncertainty Scale (IUS).20 The scale evaluates trait-like intolerance of general uncertainty. At each phase, we assessed students’ responses to medical uncertainty using the Physicians’ Reactions to Uncertainty Scale (PRUS).21,22 The 15-item scale measures (1) anxiety, (2) concerns about bad outcomes, (3) reluctance to disclose uncertainty to patients, and (4) reluctance to disclose mistakes to physicians. All items included a 7-point Likert-type response scale ranging from strongly disagree to strongly agree. We calculated mean scores for each (sub)scale.
Data Analysis
We employed hierarchical linear modeling within SPSS 26 using the General Linear MIXED function. Mixed modeling is preferred over repeated measures analysis of variance for its flexibility handling missing data and uneven time points.23 Intraclass correlations (ICC) within the null models showed significant variation existed between students for all reactions to uncertainty, thus validating our modeling of students at level 2 and their responses at each phase at level 1. We employed restricted maximum likelihood estimation methods.23 To address RQ1 and H1, we evaluated a series of models in which phase and intolerance of uncertainty at baseline were entered as covariates. We also included age and gender as control variables.
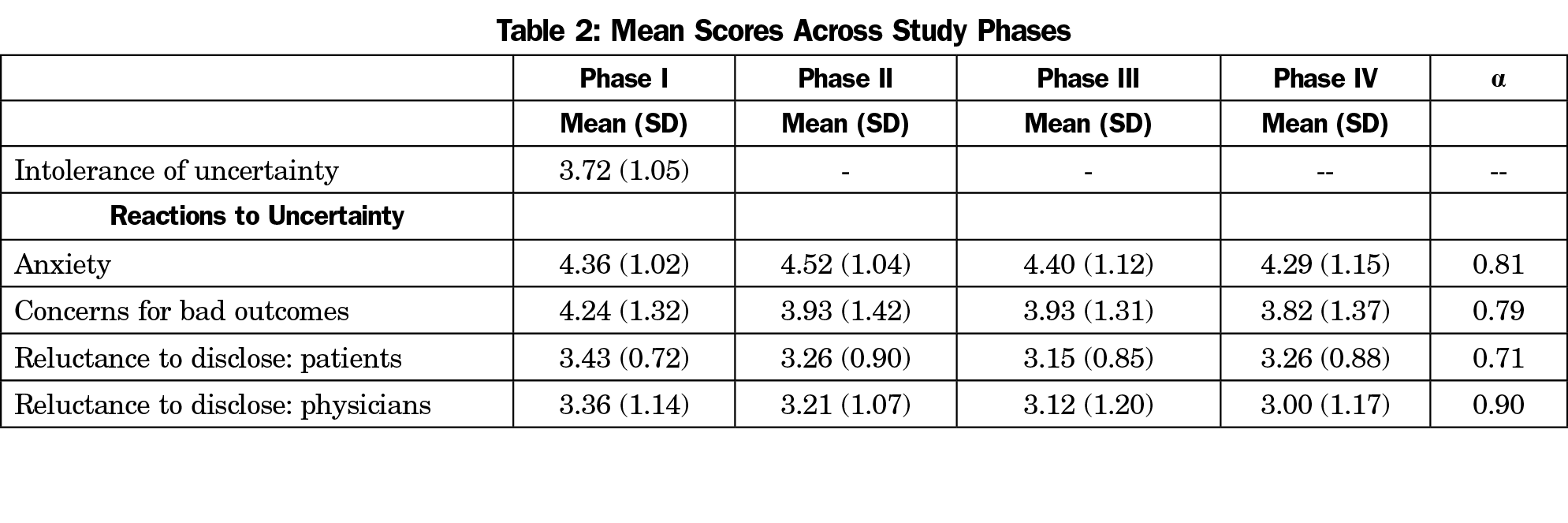
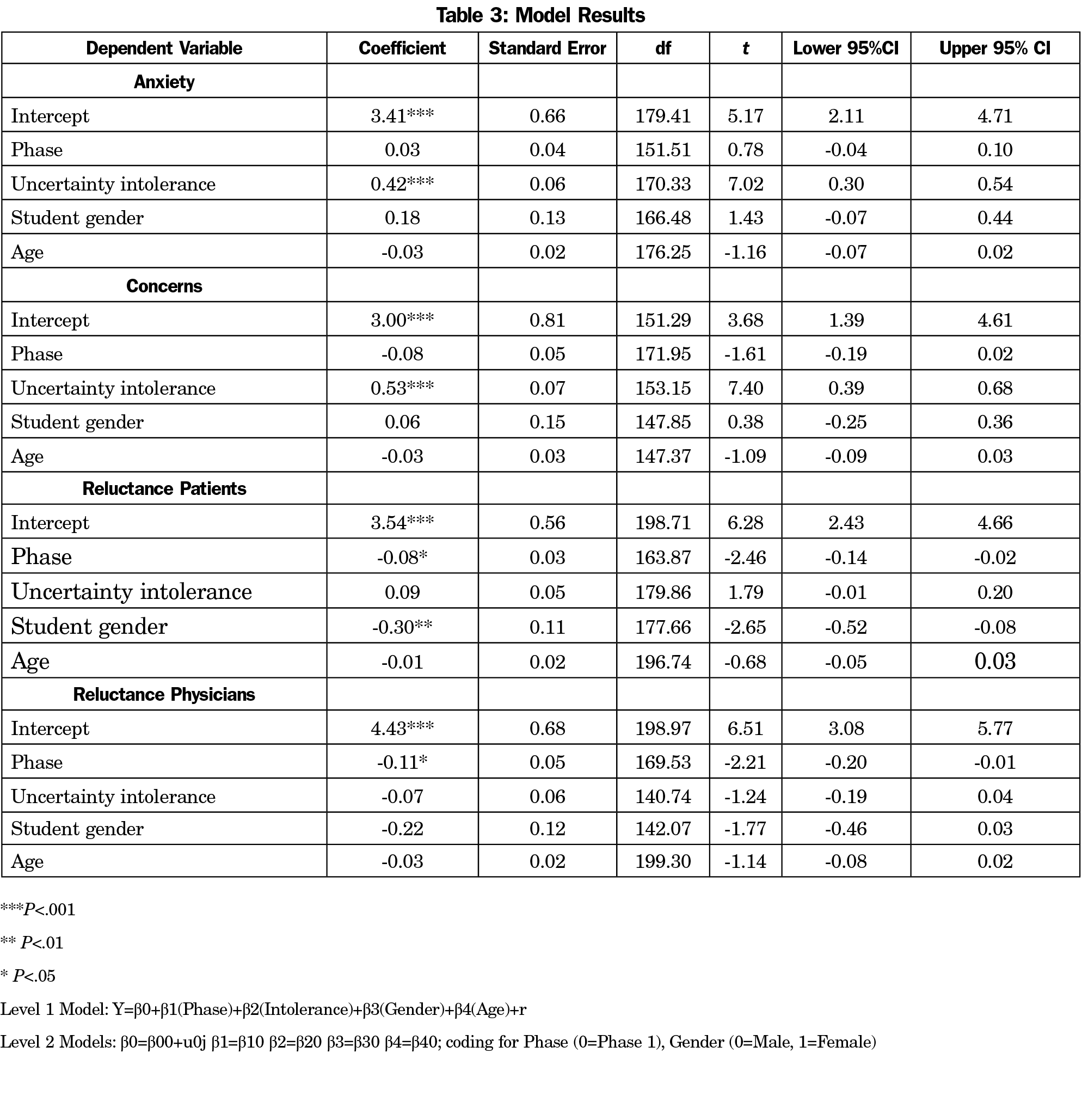
RQ1 asked how medical students’ reactions to uncertainty changed during students’ first year of clinical rotations. Table 2 shows the means for the variables at each phase and Table 3 shows model results. Students indicated somewhat strong feelings of anxiety from uncertainty at Phase I that did not significantly decrease across phases. Students reported moderate concerns about bad outcomes at Phase I that did not significantly change across phases. Students also reported at Phase I that they were not very reluctant to disclose their uncertainty to physicians or patients; still, reluctance to disclose to physicians and patients significantly decreased across phases. H1 predicted that intolerance of uncertainty would be positively associated with reactions to uncertainty. Model results showed that at each phase, intolerance of uncertainty positively predicted anxiety and concerns about bad outcomes, but not reluctance to disclose to either patients or physicians, partially supporting H1. Finally, gender predicted behavioral reactions to uncertainty, with female students significantly less reluctant to disclose uncertainty to patients than male students. Age did not predict reactions to uncertainty.
Medical educators have called for more dedicated curriculum addressing uncertainty and ambiguity in undergraduate medical education.24 Our findings suggest that students on clinical rotations would benefit from this training. In our study, students’ negative affective responses (anxiety and concerns for bad outcomes) remained stable during the first year of clinical rotations. Ideally, these negative reactions would decrease as students gain clinical knowledge and experience. The analysis revealed shifts in students’ communication in response to uncertainty as they became more willing to disclose uncertainty to patients and physicians. This finding is promising and suggests that students become more efficacious in communicating uncertainty to physicians, even if they fear making mistakes or are concerned about revealing the limits of their medical knowledge.25 Disclosing uncertainty to preceptors can prompt feedback, which is an important element of clinical education.26 The results also indicate that students become more confident in communicating uncertainty to patients, which is a central component of patient-centered care and shared decision making.27
Our results also revealed an important connection between state and trait uncertainty tolerance. Students who were characteristically less tolerant of uncertainty experienced more negative affective reactions to uncertainty in clinical encounters but did not report significantly different communication behaviors. This finding suggests that general measures of uncertainty tolerance, like the IUS,19 may reflect students’ affective reactions to uncertainty, but do not sufficiently capture students’ behavioral reactions. Hence, it may be that students high in IUS internalize their negative reactions to uncertainty but are still willing to communicate about it with patients and preceptors because they recognize the need to do so for patient care. However, the persistent negative affective reactions likely explains the connection between intolerance of uncertainty and physician depression and burnout reported in the literature.28 Students highly intolerant of uncertainty may need more assistance learning how to manage their negative reactions to mitigate these harmful outcomes. Finally, female students in this study were less reluctant to disclose uncertainty to patients than male students. However, the fact that gender did not predict other reactions to uncertainty suggests that, although there may be some individual-level differences in reactions to uncertainty, all students would benefit from curriculum designed to improve their reactions to uncertainty in patient care.
Integrating a dedicated curriculum on uncertainty in medical education could have many benefits for students entering clinical education. Teaching students to accept and even embrace uncertainty will improve their ability to make decisions when confronted with uncertainty29 and can help mitigate consequences of enduring negative reactions, including psychological distress and poor attitudes toward patients.30 Improving students’ ability to identify and manage negative reactions may also prevent harmful behavioral responses, such as decision paralysis and nondisclosure.18 Findings suggest that, as students become more willing to communicate about their uncertainty during training, educators should also explicitly teach communication skills that help students to communicate about uncertainty with preceptors and patients in a way that does not reflect poorly on them as a trainee or future medical provider.
This investigation is not without limitations. The generalizability of our findings is limited because data were collected at one institution and there was participant attrition across the four phases. Attrition may introduce bias if the students who chose not to participate in certain phases were experiencing increased levels of stress or burnout associated with uncertainty.31 Additionally, it is possible that reactions to uncertainty are associated with the amount of medical knowledge gained during clinical rotations or other student-level characteristics, inducing specialty intention. Future longitudinal research is also needed to provide a more comprehensive understanding of the connection between trait and state reactions to uncertainty. This research could shed light on how to teach students with high trait-like intolerance of uncertainty to better manage uncertainty in clinical encounters. Overall, our study confirms that more work is needed to understand how reactions shift over time from prematriculation through graduation, and how preclinical training may shape reactions during clinical education. For example, it is important to explore the role preceptors play in shaping students’ reactions to uncertainty and explore the need for faculty development in this area to increase positive role modeling.
In conclusion, our findings suggest that educators should normalize uncertainty before students begin clinical education and equip them with skills to manage negative reactions. Our results do not suggest that educators should encourage students to be indifferent to uncertainty; doing so may suppress conversations about uncertainty. We hope students maintain a healthy level of concern about patient outcomes affected by uncertainty and engage in productive behavioral responses including adaptation, deliberation, and communication.
Acknowledgments
Presentations: Preliminary analyses of the data were presented at the International Communication Association Annual Convention Virtual Meeting, May 2020, and the DC Conference on Health Communication, April 2021.
References
- Gerrity M, Earp JA, DeVellis R, et al. Uncertainty and professional work: perception of physicians in clinical practice. Am J Sociol. 1992;97(4):1022-1051. doi:10.1086/229860
- Evans L, Trotter DRM. Epistemology and uncertainty in primary care: an exploratory study. Fam Med. 2009;41(5):319-326.
- Simpkin AL, Schwartzstein RM. Tolerating uncertainty — the next medical revolution? N Engl J Med. 2016;375(18):1713-1715. doi:10.1056/NEJMp1606402
- Fox RC. Training for uncertainty. In: Merton RK, Reader G, Kendall PL, eds. The Student-Physician: Introductory Studies in the Sociology of Medical Education. Harvard University Press; 1957:207-241.
- Nevalainen M, Kuikka L, Sjöberg L, et al. Tolerance of uncertainty in medicine among 5(th) year medical students. Swiss Med Wkly. 2009;139:48S.
- Blanch DC, Hall JA, Roter DL, Frankel RM. Is it good to express uncertainty to a patient? Correlates and consequences for medical students in a standardized patient visit. Patient Educ Couns. 2009;76(3):300-306. doi:10.1016/j.pec.2009.06.002
- Kirmayer LJ. Embracing uncertainty as a path to competence: cultural safety, empathy, and alterity in clinical training. Cult Med Psychiatry. 2013;37(2):365-372. doi:10.1007/s11013-013-9314-2
- Wayne S, Dellmore D, Serna L, Jerabek R, Timm C, Kalishman S. The association between intolerance of ambiguity and decline in medical students’ attitudes toward the underserved. Acad Med. 2011;86(7):877-882. doi:10.1097/ACM.0b013e31821dac01
- Lally J, Cantillon P. Uncertainty and ambiguity and their association with psychological distress in medical students. Acad Psychiatry. 2014;38(3):339-344. doi:10.1007/s40596-014-0100-4
- Caulfield M, Andolsek K, Grbic D, Roskovensky L. Ambiguity tolerance of students matriculating to U.S. medical schools. Acad Med. 2014;89(11):1526-1532. doi:10.1097/ACM.0000000000000485
- Hancock J, Mattick K. Tolerance of ambiguity and psychological well-being in medical training: A systematic review. Med Educ. 2020;54(2):125-137. doi:10.1111/medu.14031
- Cousin G, Schmid Mast M, Jaunin-Stalder N. When physician-expressed uncertainty leads to patient dissatisfaction: a gender study. Med Educ. 2013;47(9):923-931. doi:10.1111/medu.12237
- Bhise V, Rajan SS, Sittig DF, Morgan RO, Chaudhary P, Singh H. Defining and measuring diagnostic uncertainty in medicine: A systematic review. J Gen Intern Med. 2018;33(1):103-115. doi:10.1007/s11606-017-4164-1
- Khatri A, Aung YY-M, Vijay A, Kazi S-U. Uncertainty in clinical practice: should our focus turn to medical students instead? Med Educ. 2021;55(3):413. doi:10.1111/medu.14375
- Hojat M, Vergare MJ, Maxwell K, et al. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84(9):1182-1191. doi:10.1097/ACM.0b013e3181b17e55
- Han PKJ, Schupack D, Daggett S, Holt CT, Strout TD. Temporal changes in tolerance of uncertainty among medical students: insights from an exploratory study. Med Educ Online. 2015;20(1):28285. doi:10.3402/meo.v20.28285
- Weissenstein A, Ligges S, Brouwer B, Marschall B, Friederichs H. Measuring the ambiguity tolerance of medical students: a cross-sectional study from the first to sixth academic years. BMC Fam Pract. 2014;15(1):6. doi:10.1186/1471-2296-15-6
- Hillen MA, Gutheil CM, Strout TD, Smets EMA, Han PKJ. Tolerance of uncertainty: conceptual analysis, integrative model, and implications for healthcare. Soc Sci Med. 2017;180:62-75. doi:10.1016/j.socscimed.2017.03.024
- Geller G, Faden RR, Levine DM. Tolerance for ambiguity among medical students: implications for their selection, training and practice. Soc Sci Med. 1990;31(5):619-624. doi:10.1016/0277-9536(90)90098-D
- Carleton RN, Norton MAPJ, Asmundson GJG. Fearing the unknown: a short version of the Intolerance of Uncertainty Scale. J Anxiety Disord. 2007;21(1):105-117. doi:10.1016/j.janxdis.2006.03.014
- Gerrity MS, DeVellis RF, Earp JA. Physicians’ reactions to uncertainty in patient care. A new measure and new insights. Med Care. 1990;28(8):724-736. doi:10.1097/00005650-199008000-00005
- Gerrity MS, White KP, DeVellis RF, Dittus RS. Physicians’ reactions to uncertainty: refining the constructs and scales. Motiv Emot. 1995;19(3):175-191. doi:10.1007/BF02250510
- Heck RH, Thomas SL, Tabata LN. Multilevel and longitudinal modeling with IBM SPSS. New York: Routledge/Taylor & Francis Group; 2010.
- Luther VP, Crandall SJ. Commentary: ambiguity and uncertainty: neglected elements of medical education curricula? Acad Med. 2011;86(7):799-800. doi:10.1097/ACM.0b013e31821da915
- Nevalainen MK, Mantyranta T, Pitkala KH. Facing uncertainty as a medical student—a qualitative study of their reflective learning diaries and writings on specific themes during the first clinical year. Patient Educ Couns. 2010;78(2):218-223. doi:10.1016/j.pec.2009.07.011
- Chaou C-H, Chang YC, Yu S-R, et al. Clinical learning in the context of uncertainty: a multi-center survey of emergency department residents’ and attending physicians’ perceptions of clinical feedback. BMC Med Educ. 2019;19(1):174. doi:10.1186/s12909-019-1597-8
- Politi MC, Han PKJ, Col NF. Communicating the uncertainty of harms and benefits of medical interventions. Med Decis Making. 2007;27(5):681-695. doi:10.1177/0272989X07307270
- Simpkin AL, Khan A, West DC, et al. Stress from uncertainty and resilience among depressed and burned out residents: A cross-sectional study. Acad Pediatr. 2018;18(6):698-704. doi:10.1016/j.acap.2018.03.002
- Helou MA, DiazGranados D, Ryan MS, Cyrus JW. DiazGranados D, Ryan MS, Cyrus JW. Uncertainty in decision making in medicine: A scoping review and thematic analysis of conceptual models. Acad Med. 2020;95(1):157-165. doi:10.1097/ACM.0000000000002902
- Strout TD, Hillen M, Gutheil C, et al. Tolerance of uncertainty: A systematic review of health and healthcare-related outcomes. Patient Educ Couns. 2018;101(9):1518-1537. doi:10.1016/j.pec.2018.03.030
- Cooke GP, Doust JA, Steele MC. A survey of resilience, burnout, and tolerance of uncertainty in Australian general practice registrars. BMC Med Educ. 2013;13(1):2. doi:10.1186/1472-6920-13-2




There are no comments for this article.