Background and Objectives: Virtual intrauterine device (IUD) training options can improve clinician continuing education and patient IUD access. Our objective was to evaluate a virtual, hands-on IUD training for primary care clinicians.
Methods: Training sessions occurred via video conferencing and included didactic instruction on IUD eligibility, counseling, placement, and removal. Trainers used pelvic models to demonstrate procedures for all Food and Drug Administration-approved IUDs and guided trainees during hands-on practice with IUDs. Surveys administered before and immediately after training assessed clinician satisfaction and evaluated pre-to-posttraining changes in self-rated comfort level with IUD procedures. We evaluated the changes using Wilcoxon signed-rank sum tests.
Results: Thirty-four New Mexico clinicians were trained during 29 sessions from January-June 2021. Trainees (n=32 responding to pre/postsurveys) included nurse practitioners and midwives (48%), physician assistants (28%), physicians (17%), and clinicians in training (7%). Approximately one-third (37%) had previous experience placing IUDs. Elements of training delivery were highly rated by clinicians, with all trainees successfully using the virtual platform and half indicating that they would potentially choose a virtual training over an in-person option in the future. After the training, clinicians reported significantly increased comfort with all aspects of IUD placement and removal (P≤.01).
Conclusions: An interactive, virtual IUD training model was highly rated among practicing clinicians and increased their comfort with IUD placement and removal.
Comprehensive contraceptive care includes offering a range of Food and Drug Administration (FDA)-approved methods to patients.1 However, many primary care clinicians and reproductive health specialists lack the knowledge and technical skills to offer intrauterine devices (IUDs) to eligible patients.2–6 Misconceptions about IUD safety and appropriateness for specific patient populations (ie, adolescents, nulliparous patients) leave many untrained clinicians ill equipped to offer them.3,4,7–10 Training that addresses IUD knowledge gaps and technical skills can increase patient access,11,12 especially in rural communities.5,13
Training in IUD procedures is typically conducted in person. However, other viable options are needed, as in-person training logistics are difficult for rural clinicians14,15 and provider training must continue during public health emergencies. The use of simulations in procedural training and health care education prioritizes patient safety and can mitigate demands on training hours.16,17
Few evaluations of virtual options for clinician IUD training have been conducted. A Canadian study with family medicine residents found that satisfaction, procedural knowledge, and observed skills performance were comparable when the didactic and demonstration portions of an IUD insertion training were delivered via video versus a live session; both groups practiced insertion using pelvic models.18 Our objective was to evaluate an interactive live virtual IUD training for practicing clinicians by assessing satisfaction and impact on self-rated comfort with IUD procedure skills.
Virtual Intrauterine Device Practicum
The Long-Acting Reversible Contraceptive (LARC) Mentoring Program (LMP) at the University of New Mexico (UNM) Health Sciences Center has used in-person instruction to train clinicians to provide comprehensive reproductive counseling and to insert and remove IUD and implant devices since 2016, with the goal of increasing statewide access to a range of contraceptive methods.
Starting in spring 2020, the response to the COVID-19 pandemic precluded most in-person training. In response, the LMP team developed and implemented an innovative virtual, hands-on IUD practicum in collaboration with the Beyond the Pill (BtP) program from the University of California, San Francisco.19 The virtual practicum has on-going utility in New Mexico, a geographically large, predominantly rural state.20
Prior to the virtual training, attendees were mailed a pelvic model, contraceptive device demonstration kits, IUD insertion and removal instruments, and a phone camera tripod to support visualization of the model cervix and uterus. Attendees received a 2-hour, one-on-one or small group training with an experienced reproductive health provider via Zoom. The number of trainees per session was limited to allow trainers to more effectively guide participants through hands-on procedures over Zoom. The trainer delivered a 45-minute didactic presentation reviewing IUD eligibility, counseling, placement, and removal and performed an IUD procedure demonstration using a pelvic model. The trainer then provided individualized guidance while trainees practiced loading, placing, and removing all FDA-approved hormonal and copper IUDs. After the training, the pelvic model and instruments were mailed back to UNM using a prepaid label.
Trainee Recruitment
Trainees were recruited directly by LMP via professional society listservs, clinic outreach, and at reproductive training events in a rolling manner from January 2021-June 2021. Thirty-four New Mexico clinicians (all clinicians who expressed interest) were trained during 29 sessions during that time frame.
Evaluation Design
The evaluation protocol was deemed exempt by the UNM Human Research Protections Office (#16-434). The project team used anonymous surveys administered pretraining and immediately posttraining to collect information on provider demographic and clinical characteristics, to assess learner satisfaction, and to evaluate changes in self-rated comfort level with IUD procedures. Comfort level was rated using Likert scales. Surveys were adapted from measures developed by Dodge, et al21 and reviewed for face and content validity by LMP and BtP team members. Thirty-two trainees completed both the pre- and postsurveys.
Data Analysis
We collected and managed data using REDCap software.22 We conducted analyses in SPSS Statistics (Version 27, IBM, Armonk, NY). Descriptive statistics are presented as median and interquartile range or number and percentage. We used Wilcoxon signed-rank sum tests to evaluate pre-to-post training changes, overall and stratified by previous IUD experience (yes or no) or provider status (practicing or in training). Significance is reported at the P≤.05 level.
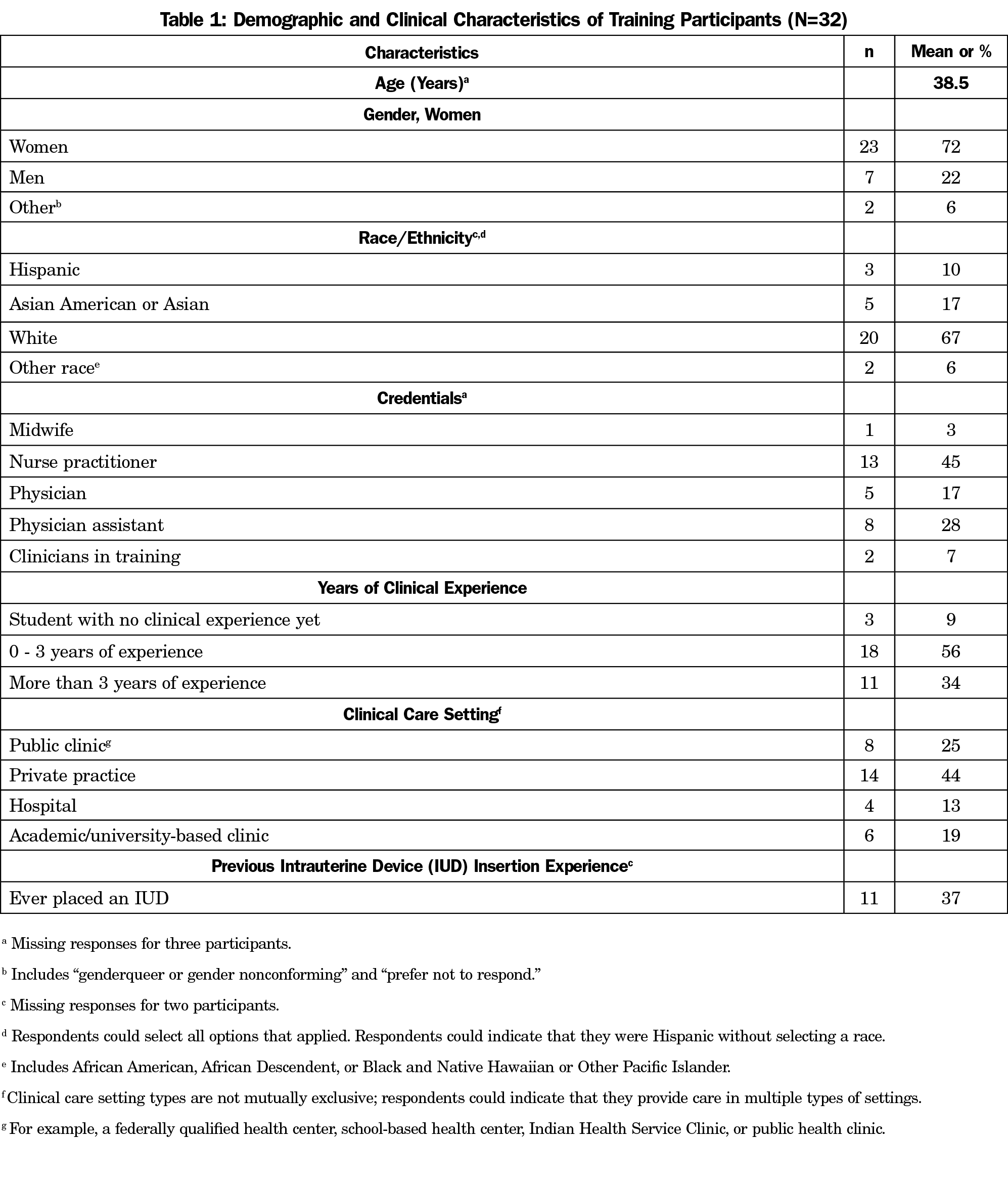
Participant Characteristics
Participating clinicians included nurse practitioners and midwives (48%), physician assistants (28%), physicians (17%), and clinicians in training (7%, Table 1). About one-third (37%) had previous experience placing IUDs.
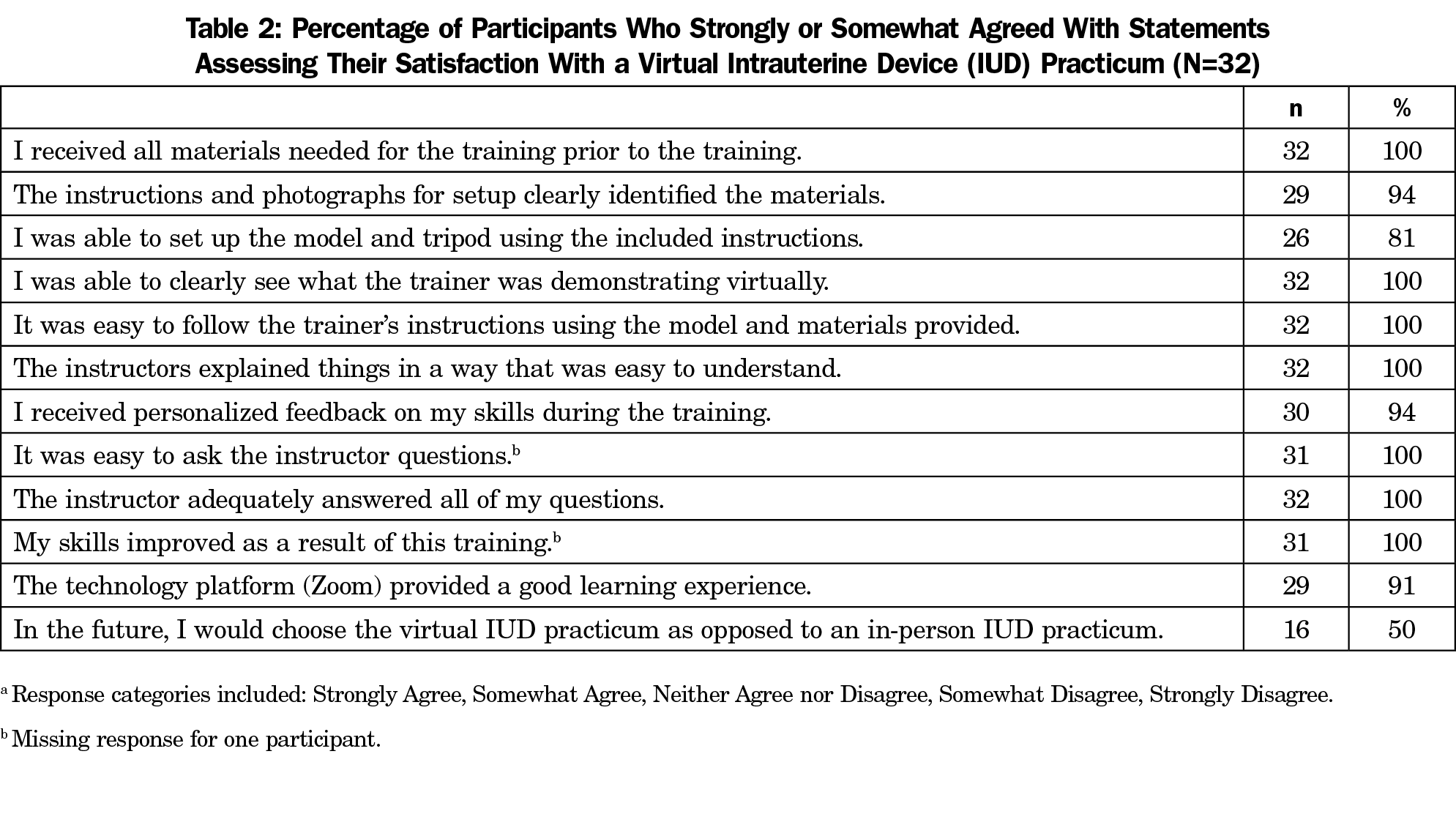
Trainee Satisfaction
Overall, elements of training delivery were highly rated, with potential room for improvement in the model and tripod setup instructions (Table 2). Half of participants said they would choose virtual over in-person training options in the future, and 100% said that they would recommend the training to a colleague. In addition, 100% of learners reported it was easy to ask the instructor questions and that their questions were adequately answered. Open-ended comments mentioned that the virtual training format simplified logistics (eg, easier scheduling, no travel time).
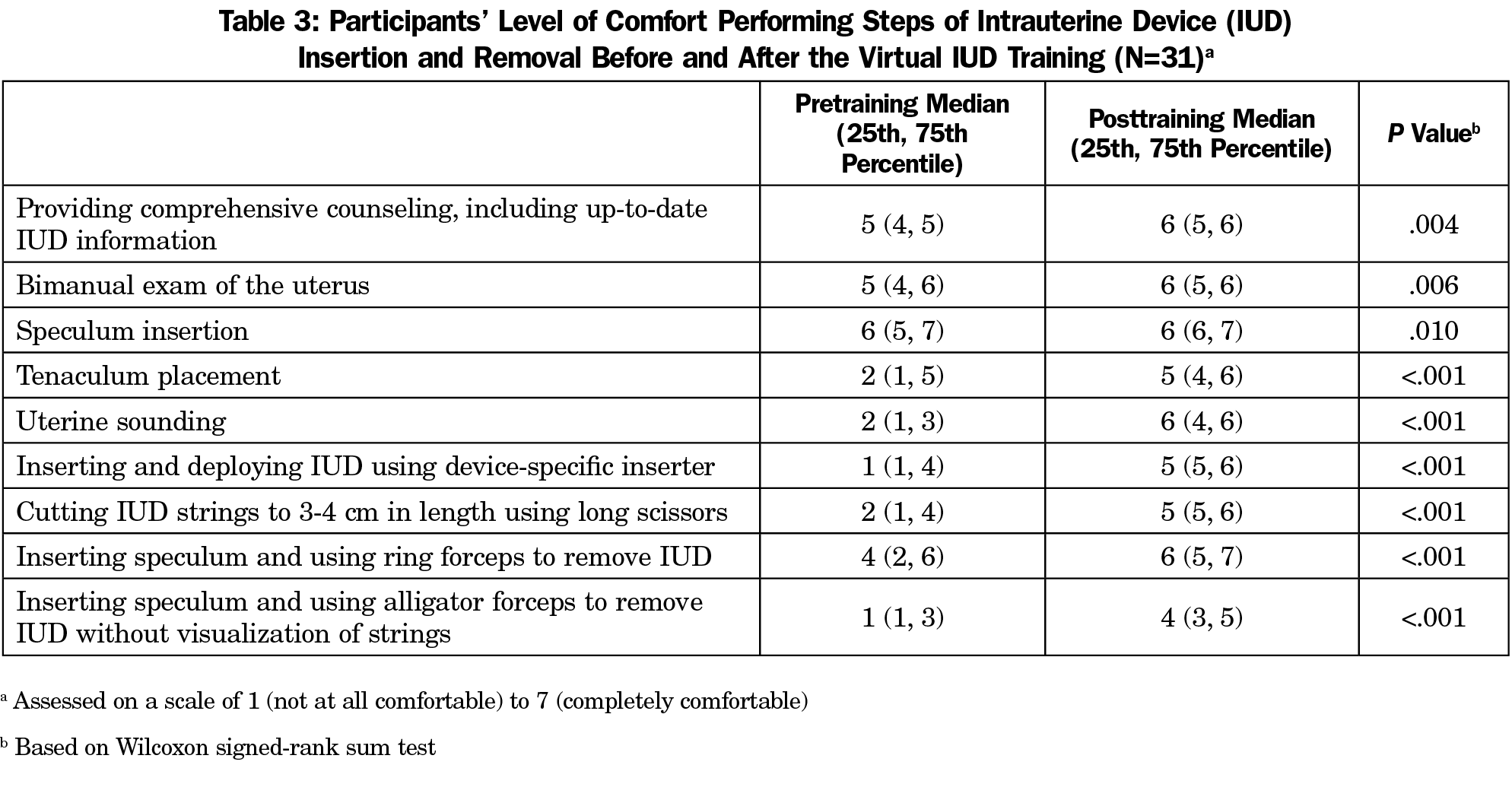
Changes in Self-rated Comfort
Participants reported statistically significant increases in comfort level with all aspects of IUD placement and removal (P≤.010, Table 3). The biggest increases in comfort pre-to-post training were reported for uterine sounding (on a scale of 1-7, pre: median 2, interquartile range [IQR] [1, 3]; post: 6 [4, 6]) and inserting and deploying IUDs (pre: 1 [1, 4]; post: 5 [5,6]). Results were consistent regardless of provider status or previous IUD experience.
Evidence generated by this model project demonstrates potential for interactive, virtual IUD skills training for clinicians. Overall, participants rated the virtual practicum highly and felt that it improved their comfort with IUD procedures, with half indicating that they would actually choose a virtual over in-person training option in the future, citing easier logistics. There are opportunities to improve the training instructions.
Similar to the video IUD module findings of Garcia-Rodriguez and Donnon,18 clinicians in this study were satisfied with an interactive live virtual IUD skills training model. Future evaluation of this model should compare outcomes for virtual versus in-person training and include objective assessment of clinician competence. In addition, outcomes for one on one versus small group training options should be compared and cost effectiveness evaluated.
Limitations of this evaluation include a small sample size and loss to follow-up (n=2). Clinicians with strong interest in online training options may have disproportionately participated, and most trainees were white women, limiting generalizability. We assessed comfort immediately posttraining, and provider perceptions may change as they apply skills in clinical practice. Social desirability bias may have influenced survey responses.
Acknowledgments
The authors are grateful to Adrien Ruvalcaba and Michelle Widener for their management of training logistics and to Whitny Schluter for her contributions to training delivery.
Financial Support for Project: Funding for this project was provided by the New Mexico Department of Health, the New Mexico Human Services Department, and The JPB Foundation. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders.
Presentations: Data included in this manuscript have previously been presented as a poster at the New Mexico Public Health Association Conference (April 2021, Albuquerque, NM) and the University of New Mexico Department of Pediatrics Research Forum (May 2021, Albuquerque, NM).
Conflicts of Interest: Jennifer Robinson and Erin Rayburn are paid Nexplanon trainers for Organon. All other authors have no conflicts of interest to disclose.
References
- Curtis KM, Jatlaoui TC, Tepper NK, et al. U.S. Selected practice recommendations for contraceptive use, 2016. MMWR Recomm Rep. 2016;65(4):1-66. doi:10.15585/mmwr.rr6504a1
- Harper CC, Stratton L, Raine TR, et al. Counseling and provision of long-acting reversible contraception in the US: national survey of nurse practitioners. Prev Med. 2013;57(6):883-888. doi:10.1016/j.ypmed.2013.10.005
- Luchowski AT, Anderson BL, Power ML, Raglan GB, Espey E, Schulkin J. Obstetrician-gynecologists and contraception: practice and opinions about the use of IUDs in nulliparous women, adolescents and other patient populations. Contraception. 2014;89(6):572-577. doi:10.1016/j.contraception.2014.02.008
- Tyler CP, Whiteman MK, Zapata LB, Curtis KM, Hillis SD, Marchbanks PA. Health care provider attitudes and practices related to intrauterine devices for nulliparous women. Obstet Gynecol. 2012;119(4):762-771. doi:10.1097/AOG.0b013e31824aca39
- Lunde B, Smith P, Grewal M, Kumaraswami T, Cowett A, Harwood B. Long acting contraception provision by rural primary care physicians. J Womens Health (Larchmt). 2014;23(6):519-524. doi:10.1089/jwh.2013.4286
- Harper CC, Henderson JT, Raine TR, et al. Evidence-based IUD practice: family physicians and obstetrician-gynecologists. Fam Med. 2012;44(9):637-645.
- Rauh-Benoit LA, Tepper NK, Zapata LB, et al. Healthcare Provider Attitudes of Safety of Intrauterine Devices in the Postpartum Period. J Womens Health (Larchmt). 2017;26(7):768-773. doi:10.1089/jwh.2016.5985
- Black KI, Lotke P, Lira J, Peers T, Zite NB. Global survey of healthcare practitioners’ beliefs and practices around intrauterine contraceptive method use in nulliparous women. Contraception. 2013;88(5):650-656. doi:10.1016/j.contraception.2013.06.005
- Berlan ED, Pritt NM, Norris AH. Pediatricians’ Attitudes and beliefs about long-acting reversible contraceptives influence counseling. J Pediatr Adolesc Gynecol. 2017;30(1):47-52. doi:10.1016/j.jpag.2016.09.001
- Murphy MK, Stoffel C, Nolan M, Haider S. Interdependent barriers to providing adolescents with long-acting reversible contraception: qualitative insights from providers. J Pediatr Adolesc Gynecol. 2016;29(5):436-442. doi:10.1016/j.jpag.2016.01.125
- Ouyang M, Peng K, Botfield JR, McGeechan K. Intrauterine contraceptive device training and outcomes for healthcare providers in developed countries: a systematic review. PLoS One. 2019;14(7):e0219746. doi:10.1371/journal.pone.0219746
- Thompson KMJ, Rocca CH, Stern L, et al. Training contraceptive providers to offer intrauterine devices and implants in contraceptive care: a cluster randomized trial. Am J Obstet Gynecol. 2018;218(6):597.e1-597.e7. doi:10.1016/j.ajog.2018.03.016
- Bornstein M, Carter M, Zapata L, Gavin L, Moskosky S. Access to long-acting reversible contraception among US publicly funded health centers. Contraception. 2018;97(5):405-410. doi:10.1016/j.contraception.2017.12.010
- Hendrickx L, Winters C. Access to continuing education for critical care nurses in rural or remote settings. Crit Care Nurse. 2017;37(2):66-71. doi:10.4037/ccn2017999
- Glazebrook RM, Harrison SL. Obstacles and solutions to maintenance of advanced procedural skills for rural and remote medical practitioners in Australia. Rural Remote Health. 2006;6(4):502. doi:10.22605/RRH502
- Sakakushev BE, Marinov BI, Stefanova PP, Kostianev SS, Georgiou EK. Striving for better medical education: the simulation approach. Folia Med (Plovdiv). 2017;59(2):123-131. doi:10.1515/folmed-2017-0039
- Ennen CS, Satin AJ. Training and assessment in obstetrics: the role of simulation. Best Pract Res Clin Obstet Gynaecol. 2010;24(6):747-758. doi:10.1016/j.bpobgyn.2010.03.003
- Garcia-Rodriguez JA, Donnon T. Using comprehensive video-module instruction as an alternative approach for teaching IUD insertion. Fam Med. 2016;48(1):15-20.
- Beyond the Pill. University of California San Francisco. Accessed October 1, 2021. https://beyondthepill.ucsf.edu/
- Metropolitan, Small Metro, Mixed Urban/Rural and Rural New Mexico Counties. New Mexico Department of Health. Accessed October 5, 2021. https://ibis.health.state.nm.us/view/docs/CHA/UrbanRuralCounties.pdf
- Dodge LE, Hacker MR, Averbach SH, Voit SF, Paul ME. Assessment of a high-fidelity mobile simulator for intrauterine contraception training in ambulatory reproductive health centres. J Eur CME. 2016;5(1):30416. doi:10.3402/jecme.v5.30416
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. doi:10.1016/j.jbi.2008.08.010



There are no comments for this article.