Background and Objectives: Burnout is associated with reduction in patient care time and leaving academic medicine, and is prevalent among faculty, residents, and advanced practice providers. Recognition may positively impact workplace well-being and reduce attrition. The objective of this study was to understand needs and preferences regarding recognition among faculty and providers in a large academic department.
Methods: A survey including quantitative and qualitative elements was sent to faculty and providers to identify whether additional recognition was needed and, if so, to seek potential opportunities to improve recognition, with mixed-methods assessment of results.
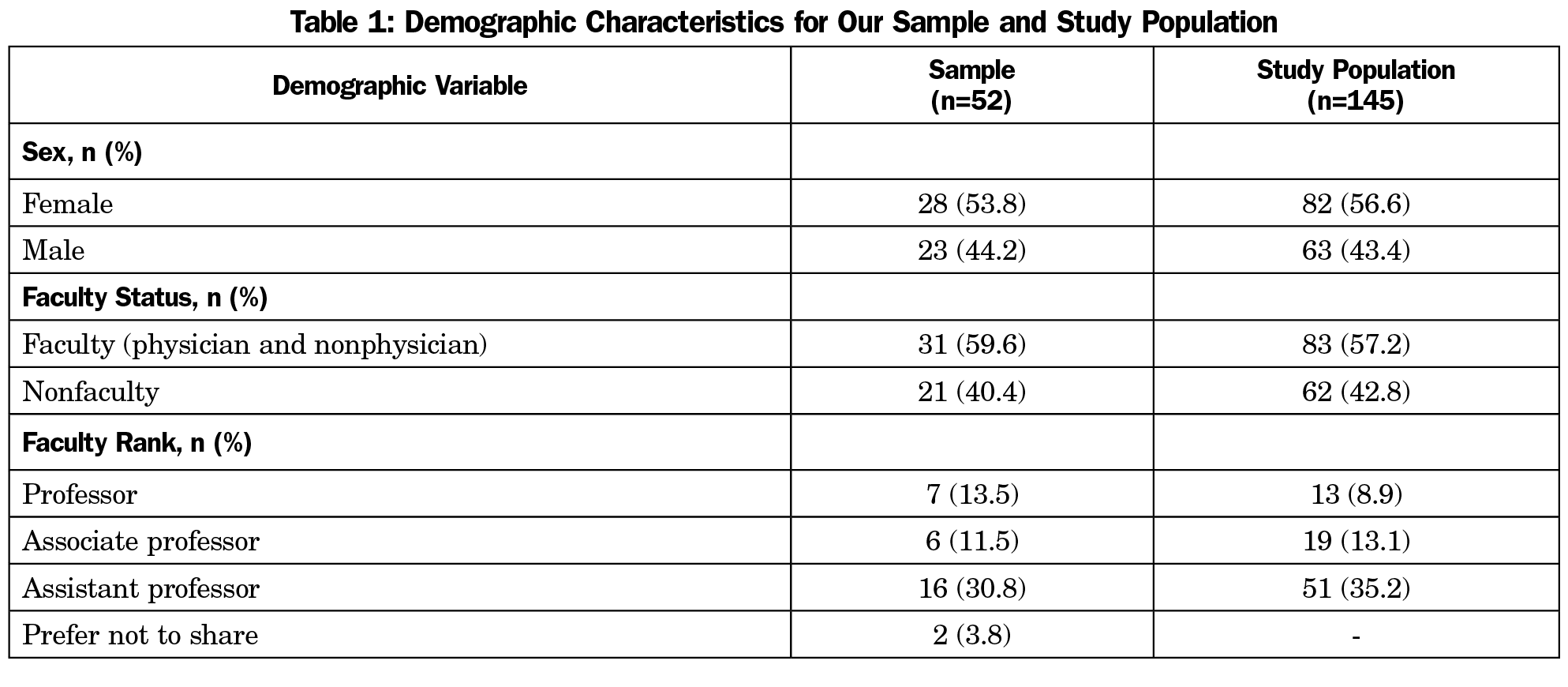
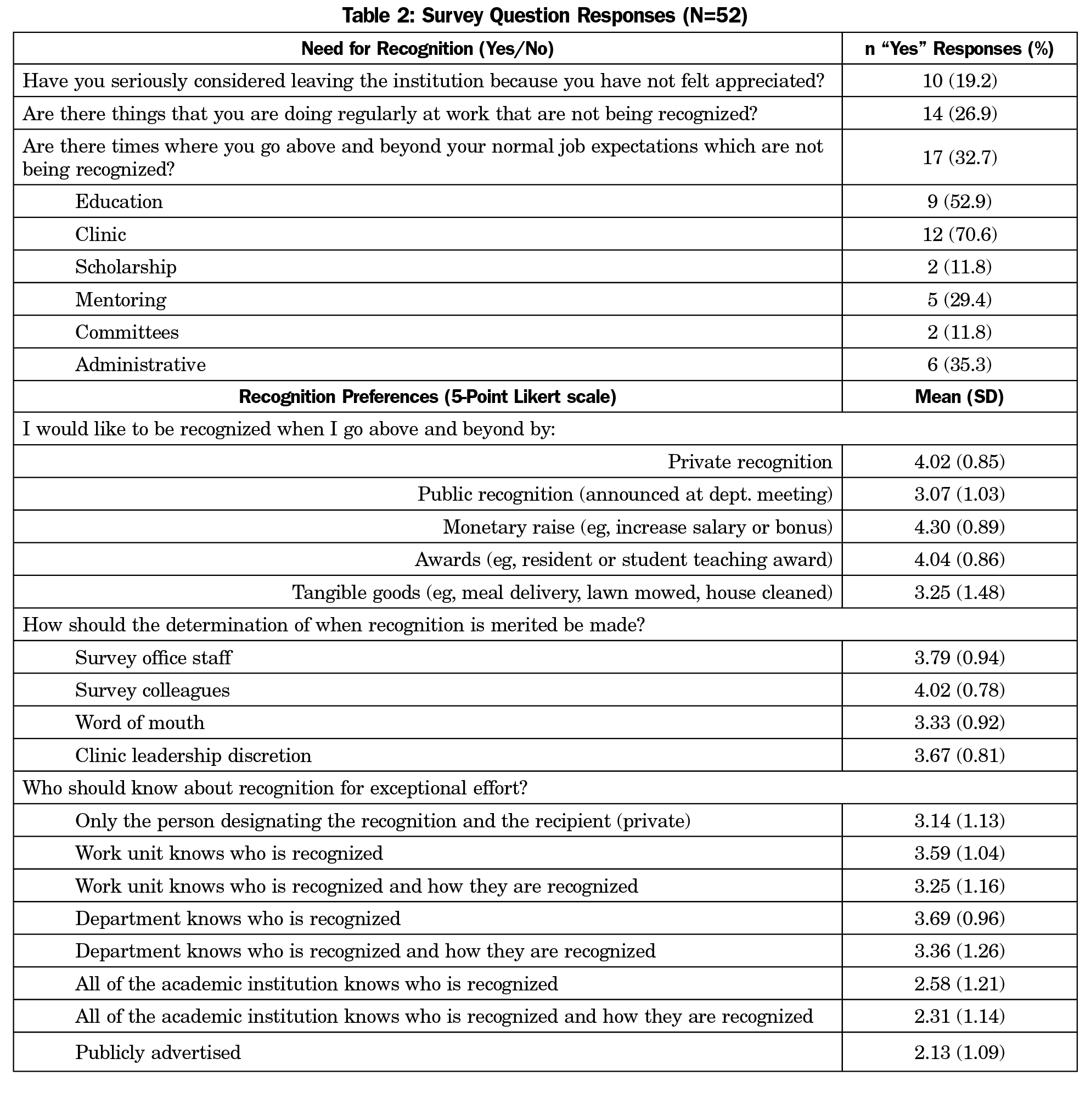
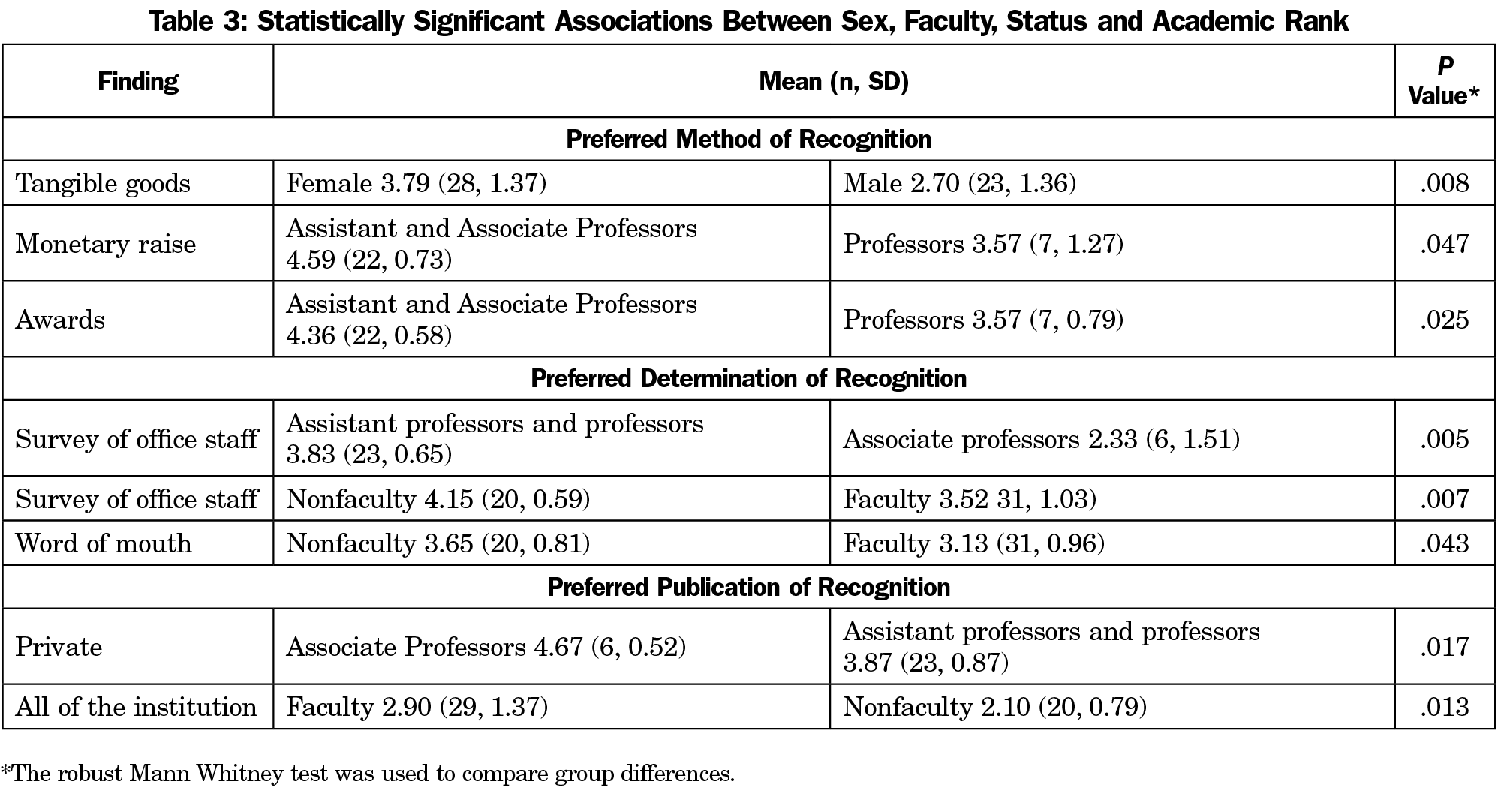
Results: Fifty-two participants completed the survey (35.9% response rate; 53.8% female, 59.6% faculty); 26.9% reported performing duties at work that are not being recognized, and 19.2% reported seriously considering leaving the institution because they did not feel appreciated. Females were more likely to want tangible goods as a source of recognition (P=.008). While providers preferred to have recommendations for recognition made by office staff (P=.007), associate professors did not (P=.005). Qualitative responses to the survey also revealed concerns regarding favoritism and risk of feeling unappreciated if a recognition system is perceived as unfair.
Conclusions: This survey demonstrated a deficit of recognition and a lack of consensus regarding how or when faculty and providers should be recognized. There were concerns regarding fairness of recognition. Efforts to enhance recognition should avoid assumptions about faculty and provider preferences, and should be attuned to fairness and inclusion.
Burnout is prevalent and associated with attrition among faculty, residents, and advanced practice providers.1,2 Insufficient recognition increases risk of burnout, and is associated with faculty leaving academic medicine.3,4 In contrast, increased recognition, feeling valued, and a sense of inclusion and connectedness have been associated with engagement, job satisfaction, and reduced turnover.2,5-8
Employee recognition is a complex construct with no single definition. Empirically distinguishable elements include achievement-based social esteem, equality-based respect, and need-based care.8 While associations have been noted between recognition, burnout, and engagement, few studies have explored related clinician preferences.9 Understanding faculty and provider recognition preferences may be useful given its potential to impact burnout and retention.
In seeking to address local levels of burnout consistent with national averages,10 our department established a mental health safety net, but efforts to reduce clinical administrative burden had been stymied. The department is geographically dispersed, making group cohesion challenging even before COVID-19-related gathering restrictions. As such, we considered exploring recognition, given its potential to build group cohesion and a sense of shared values, consistent with the equality-based respect and need-based care components of employee recognition.8
This case study explored whether there was a need for additional recognition among faculty and providers in a large academic department of family medicine, and if so, how respondents would prefer to be recognized.
Our Institutional Review Board approved this study (STUDY#11378).
Participants and Recruitment
Family and community medicine faculty, residents, and advanced practice providers at a large academic health system (n=145) were invited to take a survey via email on January 21, 2019. Participants had 2 weeks to complete it, with a reminder email sent on January 28, 2019.
Instrument
Finding no previous studies using a validated survey to evaluate recognition in the target population, we created a survey tool adhering to existing models (Supplement 1).11 Several iterations were reviewed and pilot tested by another faculty researcher in the department who provided feedback for further refinement. The survey was hosted in REDCap sofware,12 with demographics including sex, faculty status, academic rank, and clinical full-time equivalent. Other standard demographics (race, ethnicity) were not used, to allow anonymity. Survey mechanics prohibited distinguishing between residents and advanced practice providers among respondents. The survey introduction described its purpose of assessing recognition in the department, and identifying opportunities for further recognition. Survey completion time was 10-15 minutes.
Data Analysis
We analyzed quantitative outcomes using basic descriptive statistics using the R statistical program version 4.0.2 (R Foundation for Statistical Computing, Vienna, Austria) to generate reproducible statistical analyses. We performed statistical tests including Wilcoxon rank-sum test for continuous variables and a categorical response, χ2 test for categorical variables and response, and univariate regression for a continuous response. We used exploratory analysis to look for associations between sex (male vs female), faculty status (faculty vs nonfaculty), and academic rank (professor, associate professor, assistant professor). Qualitative analysis using data-driven inductive thematic analysis13 included individual coding and collaborative review of open-ended responses by authors J.A.R. and T.K.O.
Fifty-two of 145 (35.9%) faculty/providers responded. Sample and study population demographics were similar across all categories (Table 1); 14 (26.9%) respondents reported performing duties at work that are not being recognized, and 10 (19.2%) respondents reported seriously considering leaving the institution because they did not feel appreciated (Table 2).
In between-group analyses, females demonstrated a preference for recognition with tangible goods (P=.008). While nonfaculty preferred to have office staff recommend recognition (P=.007), associate professors did not (P=.005). Table 3 shows statistically significant group differences related to method, determination, and publication of recognition.
There were 84 open-ended responses from 75% of respondents (Table 4), demonstrating recognition through teaching, peer comments, patient gratitude, and intrinsic reward from meaningful work. Respondents were frequently recognized for teaching. For some, the intrinsic rewards of the work and positive comments from patients or colleagues were described as sufficient, while others expressed a lack of appreciation for going above and beyond, particularly with patient care and administrative work. There was no consensus regarding specific mechanisms by which respondents preferred to be recognized, with respondents naming many goods, services, and benefits as possibilities. These included child care, gift cards, and time off. One participant also noted, “Each individual has different needs in terms of recognition, and that can change as careers progress.”
These results support that many respondents did not feel sufficiently recognized, and reinforce the existing literature associating insufficient recognition and increased risk of attrition.14-16 The broad array of sources for recognition noted in qualitative findings reflect this construct’s many facets. Frequent teaching recognition was likely due to an institutional program for student comments on excellent teachers. While some acknowledged sufficient recognition through gratitude from patients or colleagues, many felt it was lacking. With the continuously ratcheting pressures of clinical and academic work, leaders may be unwise to rely solely on intrinsic reward to foster engagement.
No consensus emerged regarding method of identifying merit or conferring recognition. Quantitatively, differences in preference were seen based on sex, rank, and position, while qualitative findings support changing preferences through career stages. Given the disparate findings regarding preferred approach to recognition, these data suggest leaders should avoid assumptions about when and how to recognize employees.
Concerns regarding favoritism and fairness were unexpected findings. Perception of fairness in the workplace has been linked to job satisfaction and well-being.17,18 Leaders encouraging recognition should be attuned to its potential to breed favoritism and undermine well-being initiatives.
Limitations include incorporating only a single department and small sample size. Our response rate is typical for surveys regarding burnout, but there is potential for selection bias. The conditions that facilitated this inquiry in our department may not be representative of other institutions, though other large, geographically-dispersed departments may note similarities. The first survey question asked about leaving the institution due to not feeling appreciated, and it is possible that the negative tone of this question may have influenced responses to subsequent questions. As this survey was administered pre-COVID-19, attitudes may differ now. There were a few participants who crossed categories in the analysis (eg, two individuals were both faculty and advanced practice providers), but due to anonymity their data could not be corrected for, if present; in addition, residents could not be distinguished from advanced practice providers in the survey results.
Next steps may include creative approaches to addressing gaps in recognition while attending to fairness. A recognition program should both lift up individuals being recognized and fortify a healthy organizational culture. This work may provide insights for leaders attempting to reach this challenging goal.
Acknowledgments
The authors thank Jennifer Moss, PhD, for assistance in survey development.
Financial Support: This research was supported by the Penn State College of Medicine Office of Faculty and Professional Development Wellness Mini-Grant Program and the Thomas L. and Jean L. Leaman Research Endowment, Department of Family and Comunity Medicine.
Presentations: The content of this manuscript has been presented at the 2019 North American Primary Research Group (NAPCRG) Annual Meeting on November 16-20, 2019 in Toronto, Canada. It was also presented at the 2019 American Physician Health Conference in Charlotte, North Carolina.
References
- Shanafelt TD, Dyrbye LN, West CP, Sinsky CA. Potential impact of burnout on the US physician workforce. Mayo Clin Proc. 2016;91(11):1667-1668. doi:10.1016/j.mayocp.2016.08.016
- Klein CJ, Dalstrom MD, Weinzimmer LG, Cooling M, Pierce L, Lizer S. Strategies of advanced practice providers to reduce stress at work. Workplace Health Saf. 2020;68(9):432-442. doi:10.1177/2165079920924060
- Bucklin BA, Valley M, Welch C, Tran ZV, Lowenstein SR. Predictors of early faculty attrition at one Academic Medical Center. BMC Med Educ. 2014;14(1):27. doi:10.1186/1472-6920-14-27
- Lin KS, Zaw T, Oo WM, Soe PP. Burnout among house officers in Myanmar: A cross-sectional study. Ann Med Surg (Lond). 2018;33:7-12. doi:10.1016/j.amsu.2018.07.008
- Simpkin AL, Chang Y, Yu L, Campbell EG, Armstrong K, Walensky RP. Assessment of job satisfaction and feeling valued in academic medicine. JAMA Intern Med. 2019;179(7):992-994. doi:10.1001/jamainternmed.2019.0377
- Pololi LH, Krupat E, Civian JT, Ash AS, Brennan RT. Why are a quarter of faculty considering leaving academic medicine? A study of their perceptions of institutional culture and intentions to leave at 26 representative U.S. medical schools. Acad Med. 2012;87(7):859-869. doi:10.1097/ACM.0b013e3182582b18
- Condit M, Hafeman P. Advanced practice providers: how do we improve their organizational engagement? Nurse Lead. 2019;17(6):557-560. doi:10.1016/j.mnl.2019.02.004
- Renger D, Miché M, Casini A. Professional recognition at work: the protective role of esteem, respect, and care for burnout among employees. J Occup Environ Med. 2020;62(3):202-209. doi:10.1097/JOM.0000000000001782
- Angelopoulou P, Panagopoulou E. Is wellbeing at work related to professional recognition: a pilot intervention. Psychol Health Med. 2020;25(8):950-957. doi:10.1080/13548506.2019.1707239
- Shanafelt TD, West CP, Sinsky C, et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and. Elsevier; 2017:1681-1694.
- Brun J-P, Dugas N. An analysis of employee recognition: perspectives on human resources practices. Int J Hum Resour Manage. 2008;19(4):716-730. doi:10.1080/09585190801953723
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. doi:10.1016/j.jbi.2008.08.010
- Boyatzis RE. Transforming Qualitative Information: Thematic Analysis and Code Development. Thousand Oaks, CA: Sage Publications; 1998.
- Clem KJ, Promes SB, Glickman SW, et al. Factors enhancing career satisfaction among female emergency physicians. Ann Emerg Med. 2008;51(6):723-728.e8. doi:10.1016/j.annemergmed.2008.01.011
- Rizvi R, Raymer L, Kunik M, Fisher J. Facets of career satisfaction for women physicians in the United States: a systematic review. Women Health. 2012;52(4):403-421. doi:10.1080/03630242.2012.674092
- Berlanda S, Pedrazza M, Trifiletti E, Fraizzoli M. Sources of physicians’ well-being: an explorative qualitative study. TPM Test Psychom Methodol Appl Psychol. 2018;25(1).
- Leineweber C, Eib C, Peristera P, Bernhard-Oettel C. The influence of and change in procedural justice on self-rated health trajectories: Swedish Longitudinal Occupational Survey of Health results. Scand J Work Environ Health. 2016;42(4):320-328. doi:10.5271/sjweh.3565
- Hareendrakumar VR, Subramoniam S, Hussain N. Redesigning rewards for improved fairness perception and loyalty. Vision (Basel). 2020;24(4):481-495. doi:10.1177/0972262920946142



There are no comments for this article.