Background and Objectives: Family physicians play a crucial role in addressing the opioid epidemic. We studied a novel peer-review opioid prescribing educational intervention for family medicine residents that incorporates guided instruction from an interdisciplinary care team.
Methods: We used a mixed-methods study design in the setting of a family medicine residency program in the Midwestern United States. Residents participated in small group, peer-to-peer discussions of patients chronically prescribed opioids with guidance and input from faculty, a pharmacist, and pharmacy students. Discussions followed a structured approach to evaluation based on guidelines, and written recommendations were given to the patients’ resident primary care physician (PCP). For each patient, we reviewed electronic medical records to assess whether PCPs implemented the written recommendations. We used one-way analyses of variance to determine the statistical significance of changes made. The principal investigator interviewed seven participating residents to survey their satisfaction with the curriculum and collated suggestions for improvement.
Results: Over a 3-year period, we reviewed 59 patients as part of the intervention; of these, 53 had complete records reviewed for this study. Patients’ morphine milligram equivalent dosage (MME) declined modestly (P=.035). The number and proportion of recommendations implemented was correlated with the decline in MME (P=.004 and P=.013, respectively). Interviewed residents unanimously evaluated the curriculum positively, citing that the structured approach helped align their practices with guidelines.
Conclusions: The guided peer-review intervention effectively decreased chronic opioid use among patients, and residents positively evaluated the curriculum.
According to the US Department of Health and Human Services, opioid overdoses accounted for more than 42,000 deaths in 2016, 40% of which were due to prescription opioids.1 Through increased isolation, disruption of care, and social and economic instability, the pandemic has adversely impacted the preexisting opioid epidemic.2,3
Most family medicine program directors agree that chronic pain is best managed in primary care offices.4 However, opioid prescribing practices of primary care clinicians often do not align with Centers for Disease Control Opioid (CDC) Prescribing Guidelines.5,6 One family medicine residency program has demonstrated that an educational intervention utilizing guided instruction can be effective in improving residents’ guideline adherence.7,8 Other interventions have been studied in the past, but none have explored the qualitative and quantitative value of an interdisciplinary peer-review intervention in a residency program context.9-11
We developed a peer-review opioid prescribing educational intervention in a family medicine residency program, incorporating guided instruction, and examined its impact on chronic opioid prescribing practices.
The educational intervention was developed in a community-based, university-affiliated suburban family medicine residency program in the Midwest United States. Residents participated in small group, peer-to-peer discussions of patients being prescribed opioids, with faculty guidance, using a structured approach to evaluation. Patients were selected for discussion based primarily on high average monthly morphine milligram equivalent (MME) dosages over a sustained time period,* but could also be referred for review by their primary care physician (PCP) or another physician. During a typical session, two or three residents, two or three pharmacy students, a physician faculty member, and a pharmacist faculty member reviewed several patients, with one resident leading discussion of each patient. Some sessions also included a social work student and/or medical student. Residents summarized their recommendations in writing using a structured template based on CDC opioid guidelines.12 Each resident participated in one to three sessions over the course of their residency training. Written recommendations were given to each patient’s PCP, typically a resident. The PCP resident was never the direct reviewer of their own patients and did not write recommendations for their own patients.
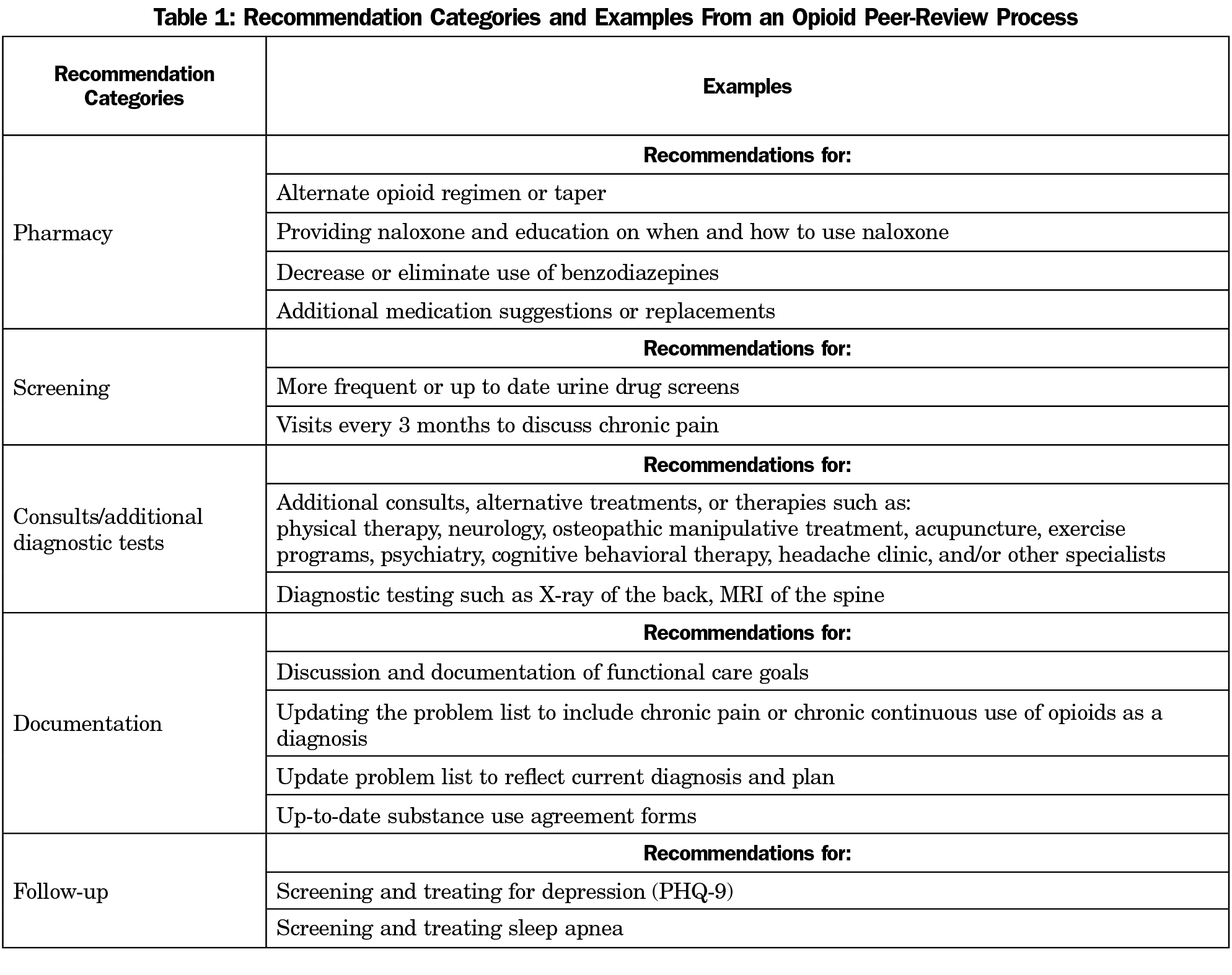
We retrospectively reviewed the written peer-review recommendations and electronic medical records (EMR) of all patients reviewed during a 3-year period (2016-2019). We then coded recommendations into categories: pharmacy, screening, documentation, follow-up, consults/additional diagnostic testing (Table 1). We evaluated each recommendation to determine whether it was followed by the PCP based on data in the EMR. Within each category, we calculated a ratio of recommendations followed to recommendations made. We used one-way analysis of variance (ANOVA) to compare the ratios across categories. We calculated the MME dosage for each patient, just before the intervention and 6 months after. We calculated change in MME using one-way ANOVA.
We recruited residents involved in recent sessions to participate in one-on-one, in-depth interviews using a semistructured approach. The purpose of the interviews was to assess residents’ satisfaction and self-reported learning from the peer-review process, in both reviewer and PCP role; identify barriers to implementation of recommendations; and identify areas for improvement. We invited residents to interview with several email solicitations, and all those who responded were interviewed. Interviews were conducted either in-person or by videoconference. The principal investigator (L.A.), a neutral interviewer, recorded, transcribed, and coded each interview in detail, using a conventional content analysis approach.13 The investigator was supervised by a senior researcher with qualitative research experience (J.P.). This study was approved by the institutional review boards of Michigan State University and Sparrow Clinical Research Institute.
We reviewed care of 53 patients; an additional five patients were excluded due to incomplete data in the data analysis tool. Patients were most likely to be female, middle-aged, and White, non-Hispanic (Table 2).
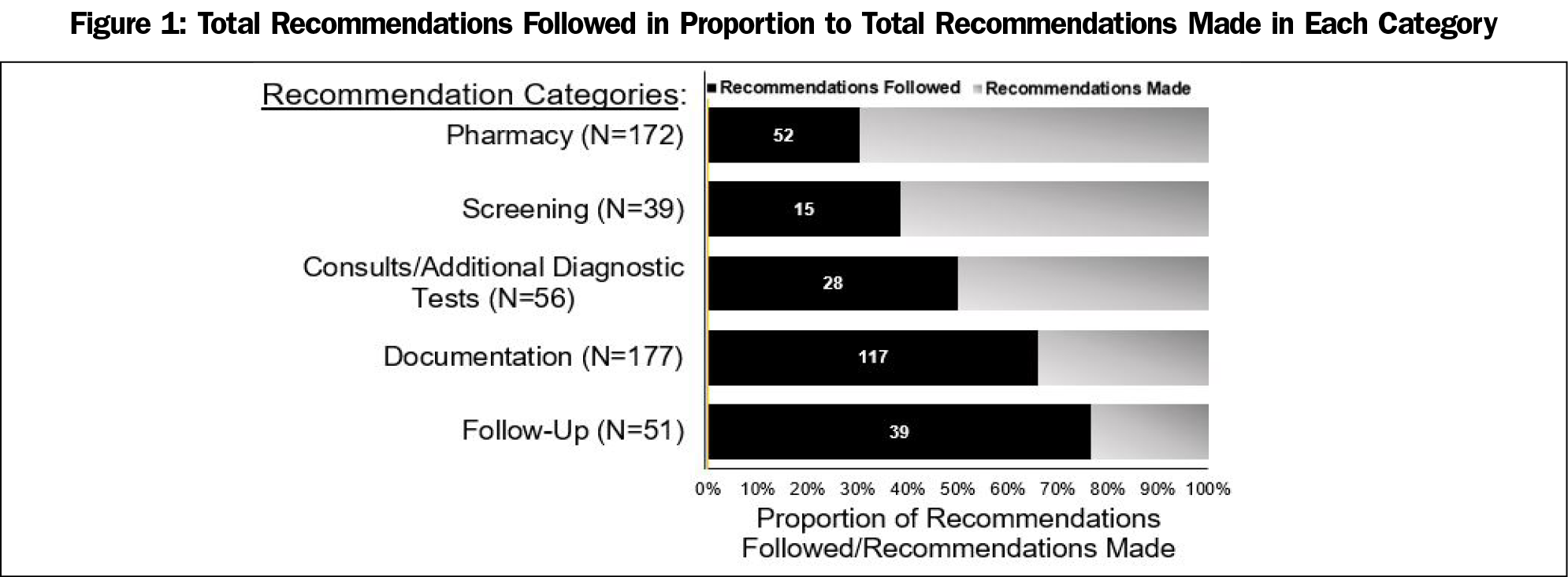
Across all patients, a total of 514 recommendations were made (average 10 recommendations per patient). Physicians were more likely to adhere to documentation recommendations than to screening, pharmacy, and consult/additional diagnostic testing recommendations (P<.05; Figure 1). We were encouraged to see that the overall, average MME decreased modestly, from 147.75 (SD=243.93) to 133.05 (SD=235.95); P=.035. Both the total number of recommendations followed and the proportion of recommendations followed were correlated with a decrease in MME (P=.004 and P=.013, respectively).
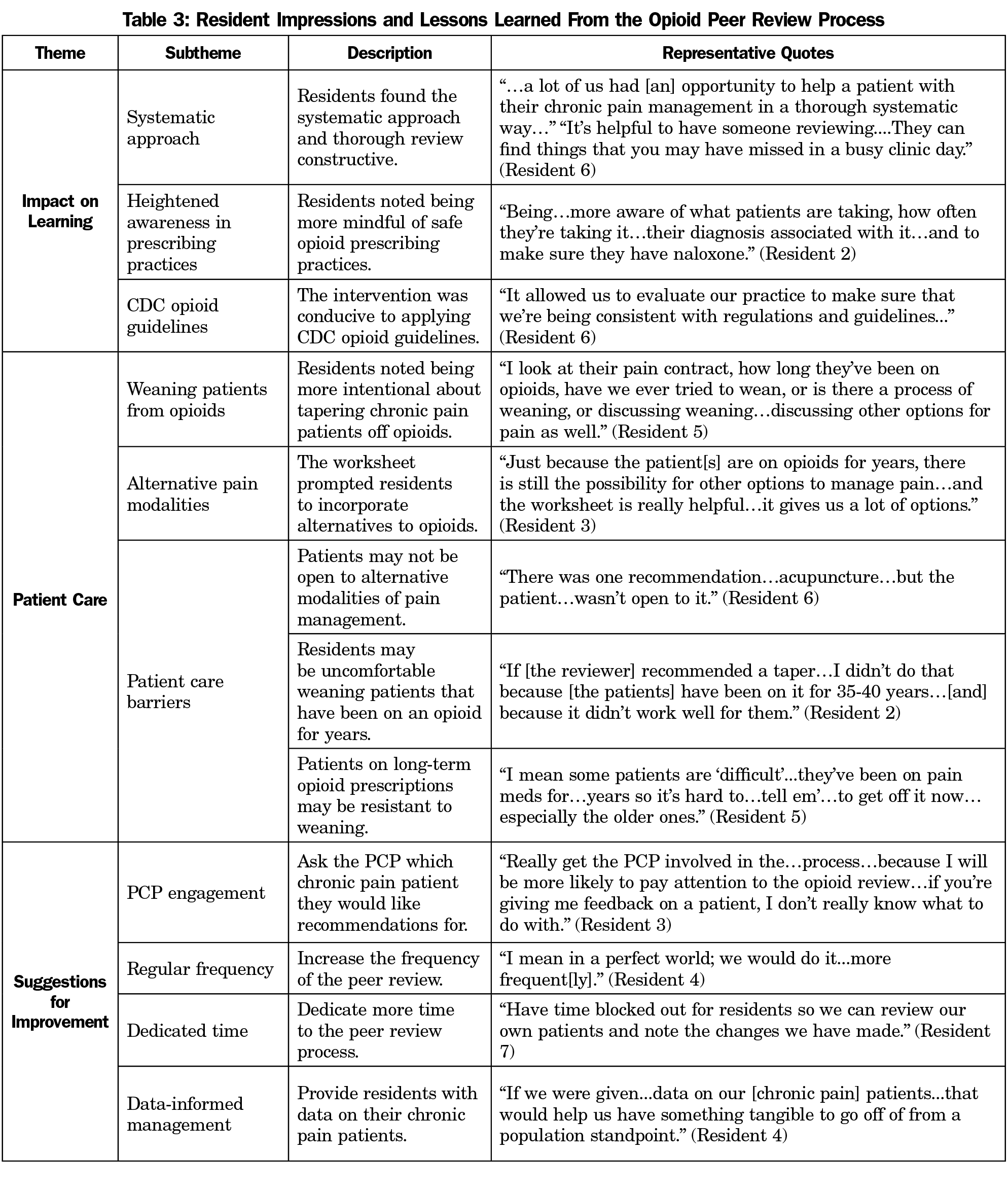
Of 32 eligible residents, seven participated in interviews. Prior to the interactive peer-to-peer exercise, residents primarily received education on opioid management in traditional lecture-based format. Residents reported that peer-review sessions attuned them to safer opioid prescribing practices: incorporating periodic pain contracts, ordering urine drug screens, investigating alternative therapies, conducting a comprehensive review of the patient’s problem list and history, and following documentation protocols. They reported better awareness of CDC guidelines and appreciated the systematic approach (Table 3). Residents particularly noted that the pharmacist and pharmacy students enhanced learning by suggesting specific dosages or medication substitutes.
Residents found the recommendations useful when applied to their own patients, prompting them to initiate decreasing opiate dosages and recommending alternative therapies. Several residents incorporated naloxone prescribing into their practice because of the peer-review intervention. However, they also experienced barriers to implementation, including patient resistance to decreasing doses. Some residents had discomfort initiating discussions about tapering with patients who had been on opioids for decades.
Residents recommended suggestions for improving the peer-review process, including encouraging PCPs to select patients for review, provision of the PCP with more comprehensive data about their patient panels, more frequent peer review, and more time for implementation of peer review. One resident stated participating in a second session would increase their understanding of CDC opioid guidelines.
All seven residents interviewed reported that the peer-review process was an effective use of time and indicated a desire to continue the curriculum. One resident noted that the intervention template could be applied to other guided interventions to improve patient care.
This residency-wide intervention combining didactic guided instruction and interdisciplinary peer-to-peer discussion had a positive impact on opioid prescribing practice for reviewed patients, particularly when PCPs were able to successfully implement recommendations. Residents who participated in qualitative interviews unanimously had a positive impression of the opioid peer review process, citing that the systematic approach helped to heighten their awareness of best practices for opioid prescribing. Next steps for the study could include screening patients for opioid use disorder and offering appropriate treatment, as well as utilizing additional resources or role-playing to simulate challenging patient discussions.14
Limitations of our study include a small sample size and evaluation of the intervention within a single residency program. Additionally, since the MME was taken as a snapshot of 1-month postintervention and at 6 months, long-term patient outcomes are not known. The size of the educational intervention did not permit evaluation of patient-oriented outcomes, such as premature death.
In conclusion, an interdisciplinary, guided peer-review intervention proved to be an asset in resident instruction and implementation of CDC opioid guidelines.
High average monthly MME defined as >50 MME/day for >90 days and/or patients prescribed opioids and benzodiazepines concurrently.
Acknowledgments
Financial Support: Financial support was provided by the Department of Family Medicine of Michigan State University College of Human Medicine.
Presentations: This study was presented at the 48th North American Primary Care Research Group Annual Meeting (Virtual), November 23, 2020; and
2021 Society of Teachers of Family Medicine Annual Spring Conference, May 3-5, 2021 (virtual).
References
- What Is the US Opioid Epidemic? US Department of Health and Human Services. 2021. Accessed December 2, 2021. https://www.hhs.gov/opioids/about-the-epidemic/index.html
- Weiner S. COVID-19 and the opioid crisis: When a pandemic and an epidemic collide. Association of American Medical Colleges. July 2020. Accessed July 27, 2020. https://www.aamc.org/news-insights/covid-19-and-opioid-crisis-when-pandemic-and-epidemic-collide
- Wan W, Long H. ‘Cries for help’: Drug overdoses are soaring during the coronavirus pandemic. The Washington Post. July 1, 2020. Accessed December 1, 2021. https://www.washingtonpost.com/health/2020/07/01/coronavirus-drug-overdose/
- Zoberi K, Everard KM. Teaching chronic pain in the family medicine residency. Fam Med. 2018;50(1):22-27. doi:10.22454/FamMed.2018.134727
- Khalid L, Liebschutz JM, Xuan Z, et al. Adherence to prescription opioid monitoring guidelines among residents and attending physicians in the primary care setting. Pain Med. 2015;16(3):480-487. doi:10.1111/pme.12602
- Thibodeaux AM, Foster KC, Skelley JW, Sims M. Opioid prescribing habits in a family medicine residency program for the management of non-cancer pain. Innov Pharm. 2019;10(2):10. doi:10.24926/iip.v10i2.1149
- Austin RC, Fusco CW, Fagan EB, et al. Teaching opioid tapering through guided instruction. Fam Med. 2019;51(5):434-437. doi:10.22454/FamMed.2019.502509
- Coon SA, Hill LG, Hutchison RW, et al. Mobilizing pharmacists to address the opioid crisis: A joint opinion of the ambulatory care and adult medicine practice and research networks of the American College of Clinical Pharmacy. J Am Coll Clin Pharm. 2020;3:1493-1513. doi:10.1002/jac5.1331
- Fujita AW, LaRosa A, Carter A. Treating withdrawal and pain in inpatients with opioid use disorder: a brief educational intervention for internal medicine residents. MedEdPORTAL. 2021;17:11123. doi:10.15766/mep_2374-8265.11123
- Lagisetty, P., Klasa, K., Bush, C., Heisler, M., Chopra, V., & Bohnert, A. (2017). Primary care models for treating opioid use disorders: What actually works? A systematic review. In PLoS ONE (Vol. 12, Issue 10). doi:10.1371/journal.pone.0186315
- Arizmendez NP, Kotovicz F, Kram JJF, Baumgardner DJ. Multimodal local opioid prescribing intervention outcomes in chronic noncancer pain management. J Am Board Fam Med. 2019;32(4):559-566. doi:10.3122/jabfm.2019.04.180296
- Calculating Total Daily Dose of Opioids for Safer Dosage. Centers for Disease Control and Prevention. Published 2008. Accessed September 10, 2020 https://www.cdc.gov/drugoverdose/pdf/calculating_total_daily_dose-a.pdf
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277-1288. doi:10.1177/1049732305276687
- Scope of Pain, Safer/Competent Opioid Prescribing Education Micro-cases. Boston University School of Medicine. Published 2021. Accessed Sept 22, 2021. https://www.scopeofpain.org/micro-cases/




There are no comments for this article.