Background and Objectives: Little is known about how comfort with uncertainty (CwU) influences career choice in medical students. The authors of this study examined the correlation between CwU and primary care career choice.
Methods: In academic years 2017-2018 and 2018-2019, the authors distributed surveys to third-year medical students from eight US medical schools, seven in Texas. The survey tool included two CwU scales and one comfort with ambiguity scale. Other questions covered career plans, family and personal background, and student debt. In the subjects’ fourth year of medical school, authors obtained match data from the medical schools and the authors further communicated with the students where indicated. The primary outcome was the composite score of the three scales correlated to career choice, with a focus on primary care and family medicine.
Results: Among 642 participants, there was no difference in CwU scores between students who matched into primary care versus specialty fields (3.39 vs 3.37 average of three scales, P=.65, each individual scale NS) or family medicine (FM) vs all other fields (3.39 vs 3.37 average of three scales, P=.81). Other bivariate predictors of FM choice were more similar than different to previous studies, such as osteopathic more likely than allopathic, lower family income, planning to care for underserved populations, and had a primary care role model. Logistic regression found the two biggest predictors of FM were osteopathic training and the importance of educating patients about health promotion and disease prevention.
Conclusions: We found no correlation between CwU and medical student career choice for primary care or FM. We discuss confounding factors that may impact results, as well as recommendations for medication education and public policy.
Comfort with uncertainty (CwU) has been recognized as important to primary care practice globally.1-4 Commentators have recently called for an increasing tolerance of uncertainty across all US physicians, recognizing its association with improved health care quality and costs.3,5 Less is known about how and when physicians develop this comfort.
The problem of uncertainty in medicine has been described as “… simply too complex – and the research enterprise too vast – to consolidate within one unified research program or theoretical paradigm.”6
The most commonly used scale in this literature for physician uncertainty (by Gerrity et al) is comprised of four domains: anxiety due to uncertainty, concern about bad outcomes, reluctance to disclose uncertainty to patients, and reluctance to disclose mistakes to physicians.7 Beresford described uncertainty as inadequate technical or procedural knowledge, not knowing patients’ wishes, and difficulty applying abstract criteria to concrete situations.8 Nevalainen et al found that third-year medical students’ uncertainty is associated with insecurity about professional skills, a realization that medicine is often inexact, and an awareness of the responsibility associated with patient care.9
CwU in physicians has been associated with increased job satisfaction, decreased work stress, and decreased risk of burnout10, 11; broader scope of practice12; less excessive testing13,14; less unnecessary treatment15; fewer delays in care and episodes of patient harm16 ; greater patient engagement17; and decreased total patient care charges.18 This comfort is especially crucial in primary care, as many patient concerns are undifferentiated, unorganized, and often do not lead to a single organic diagnosis.19-22 An analysis of audio recordings of patient visits to general internists in the United States found that 71% included verbal expressions of uncertainty to patients.23
Previous research has found mixed results of the association between CwU and medical student career choice. Nevalainen et al found that medical students in Finland who reported poor comfort with uncertainty were more likely to express a belief that a general practitioner’s career was too challenging.4 A study conducted in the 1980s found that intolerance of ambiguity was not found to be predictive of specialty choice.24 Others found intolerance of uncertainty related to avoiding family medicine (FM), geriatrics, and psychiatry.24-26
The purpose of this study was to examine the association between CwU and specialty choice in medical students, particularly regarding FM and primary care. We also examined the relative contribution of the influence of CwU on FM choice in the context of other known predictors.
We surveyed medical students on the first day of their required third-year FM clerkship, in most cases. This timing minimized their exposure to FM before they answered survey questions. The survey instrument included the short form versions of scales measuring comfort with uncertainty: the Physicians’ Reactions to Uncertainty Scale (PRUS),27 the Need for Closure scale (NfC),28 the Tolerance for Ambiguity (TfA)29 scale, and other features known to correlate with the choice of FM or primary care as a career, including rural upbringing; parental education; interest in research; and many other factors. There were no incentives for participation.
Our survey instrument is shown in Appendix 1 (https://journals.stfm.org/media/5036/young-appendix1.pdf). Socioeconomic status was self-reported by the participant as one of five categories. Student loan debt was self-reported by free text and included undergraduate and medical school expected debt at graduation. The instrument mostly contained the questions of the three uncertainty scales and other questions based on previous studies of medical student interest in family medicine and primary care. Other major subsections included premedical school life, career objectives, and other basic demographics. The instrument went through several rounds of edits by participating RRNeT faculty members and was piloted for content and clarity to noneligible students at the primary investigator sites.
We approached students each rotational block over the academic year 2017-2018 and 2018-2019 in medical schools that send students to work with participating residencies of the Residency Research Network of Texas (RRNeT). Texas medical schools are required to have a 1-month family medicine rotation in the third year. There were three exceptions to this. Two of the RRNeT schools were in the process of converting to a compressed curriculum, so some second-year students were included at those sites. Students of the Uniformed Services University of the Health Sciences (USUHS) begin core clerkships during January of the second year of medical school through December of the third year, which include a required 5-week family medicine rotation. We excluded students from our analyses if they did not participate in the match in their normal fourth year or did not match.
For the seven Texas medical schools, we obtained match data from each school’s dean’s office to determine where each student matched for residency in the spring of their fourth year (with permission of the students obtained when they filled out the survey instrument). For students matching in an internal medicine or pediatrics residency, we contacted them individually to ascertain whether they intended to have generalist or specialist careers. For USUHS students, we sent a follow-up survey to the subjects in the spring of their fourth year. For nonrespondents, we followed up at the dean’s office. We collected data from the medical schools after the Supplemental Offer and Acceptance Program (SOAP) process.
Each of the CwU scales is a Likert-type format. For each question, we calculated means, subscale, and overall score for both substudies. The primary outcome was whether CwU was an independent predictor of primary care specialty choice. There was very little missing data in the completed surveys. Respondents who filled out some of the survey, but none of the uncertainty scales, were counted as nonresponders and were not analyzed. A few surveys had a single missing response in one of the uncertainty scales. Since a zero in that space would have an oversized impact on the final scale score, those values were imputed by transferring answers from similar questions in other parts of the instrument. For example, if the respondent answered “I find the uncertainty in patient care disconcerting,” but not “Uncertainty in patient care makes me uneasy,” we imputed the score from the answered question into the blank one (.06% of these cells had missing data). Other missing data elements were not imputed and left blank. We analyzed categorical data using χ2. We analyzed continuous data, including Likert scales, using Student’s t test. We calculated bivariate correlation coefficients to identify variables that were associated with specialty choice. We included those that had a P value of <.20 to identify independent predictors of specialty choice. We used backwards stepwise regression to construct a parsimonious model. We looked at a subset of models, and eliminated one variable with the lowest P value at a time until no variables remained in the model. We assessed multicollinearity of independent variables by calculating values for tolerance and the variance inflation factor (VIF). Values for tolerance >0.2 and for VIF <5 were considered as being compatible with a low collinearity.
Statistical Package for the Social Scientist (SPSS) version 26 was used for analysis (SPSS Inc, Chicago, IL). All tests were 2-tailed, and we set a levels at 0.05 to determine statistical significance.
Approval for this study was obtained from Institutional Review Board of UT Health San Antonio and each participating residency site, if required.
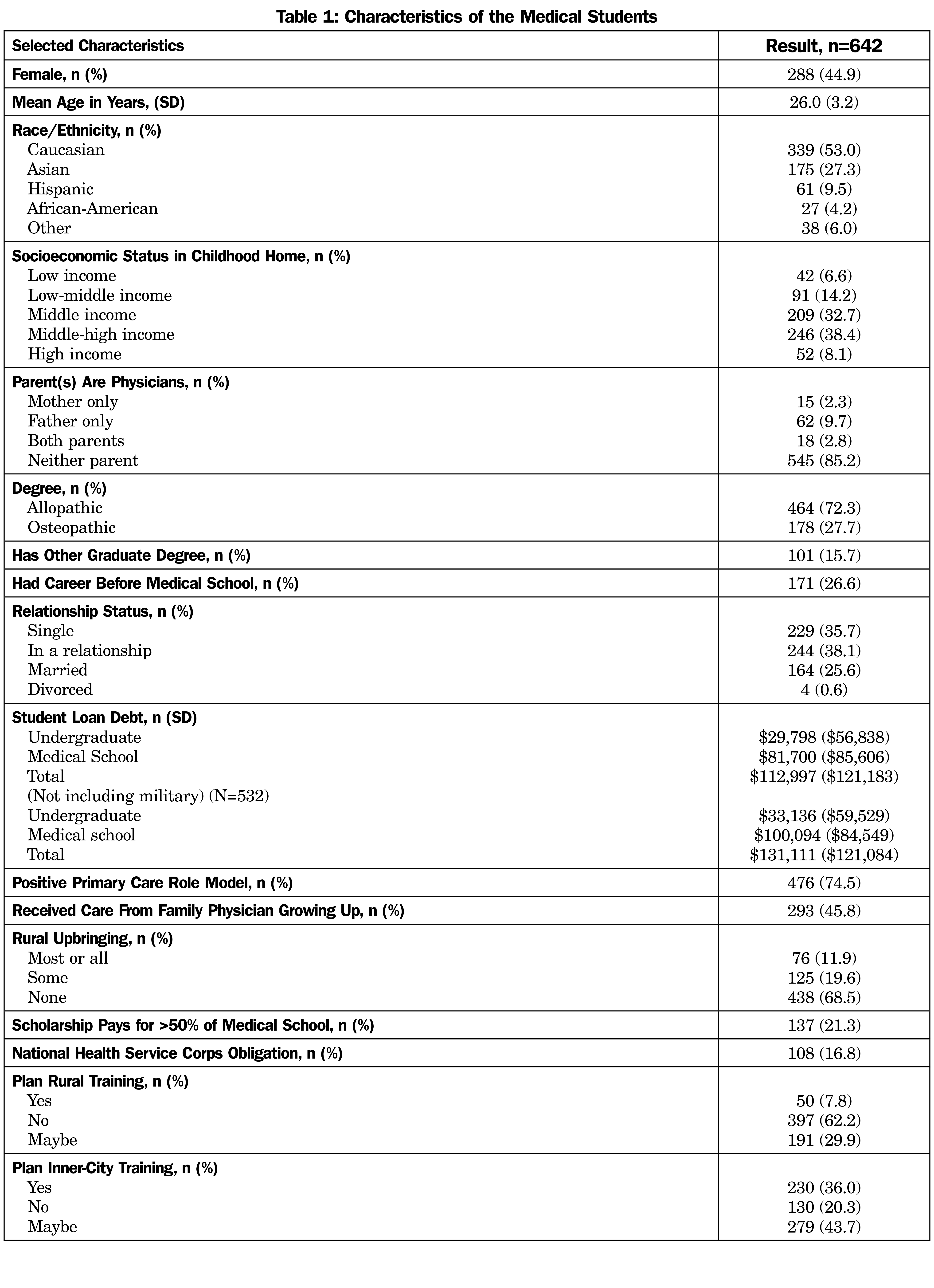
We approached 785 medical students, and 658 (83.8%) initially participated. We obtained match data on 642 students (97.7%). The other 16 students did not fill out the uncertainty scales, did not match, or chose not to participate in the match (they were still working on their PhD, for example) and were excluded from further analysis. Demographic characteristics of the students who participated are shown in Table 1.
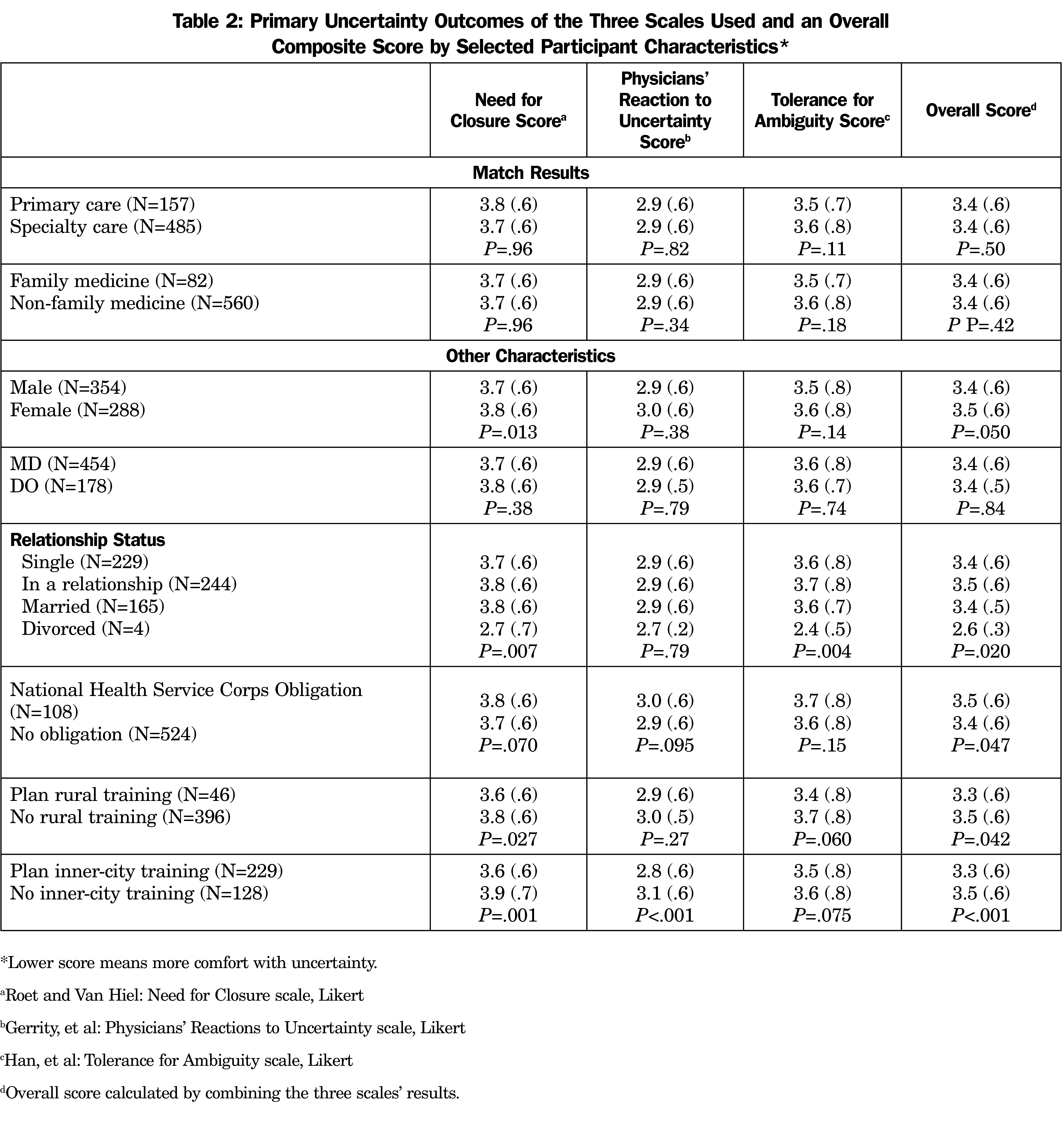
There was no difference in the CwU composite score between students who matched into primary care versus specialty fields (3.4 vs 3.4 average of three scales, P=.65, each individual scale NS) or FM vs all other fields (3.4 vs 3.4 average of three scales, P=.81, Table 2; lower scores represent more CwU). Characteristics that did show an increase in CwU included male gender (3.4 vs 3.5, P=.050 for composite score), not having a National Health Service Corps scholarship (3.4 vs 3.5, P=.047), planning rural training (3.3 vs 3.5, P=.04), and planning inner-city training (3.3 vs 3.5, P<.001). Some characteristics not associated with CwU included race/ethnicity (P=.077), student loan amount (P=.18), medical school site (P=.085), or degree type (P=.93) by the composite measure, nor any of the three individual CwU scales. There were no differences in these outcomes by the time within the academic year the student was on the family medicine rotation or which other rotations they had completed. There were no significant differences in career outcomes when the question about their intended career choice from their third-year survey was used (vs what they actually matched in).
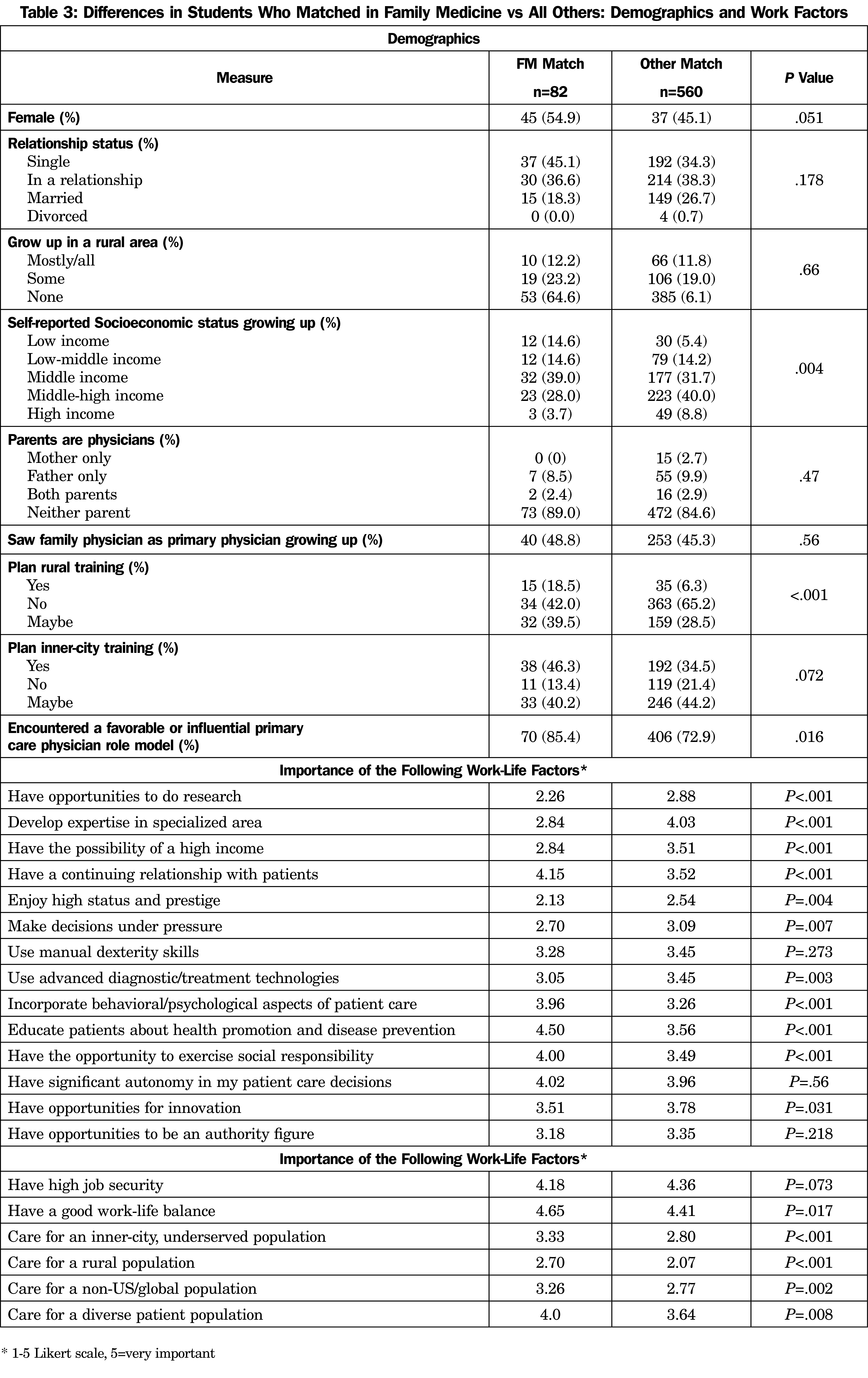
Other predictors of FM choice included osteopathic students more likely than allopathic (35/177 [19.8%] vs 47/464 [10.1%], P=.001), lower household income growing up (measured over five categories, P=.004), planned rural training (yes or maybe 47/81 [58%] of FM vs 194/557 [35%] other specialties, P<.001), had a primary care role model (53/62 (85.5%) FM vs. 275/378 (72.8%) other specialties, P=.033), and race/ethnicity (range 0% African American to 24.6% Hispanic, P=.003).
Other factors that predicted choosing FM, as measured by a 1-5 Likert scale, are shown in Table 3. Especially notable are the importance to the FM match students of a work life that includes continuous patient relationships, psychological/behavioral aspects of care, educating patients, social responsibility, caring for inner-city populations, caring for rural populations, caring for non-US populations, and caring for diverse populations. Of less importance to FM match students were research, expertise in a specialized area, high income, status/prestige, and using advanced technologies.
Notable factors that did not predict FM choice included upbringing in a rural community (P=.66), parents are physicians (P=.47), and student loan debt (P=.23, the result is the same if the military match is excluded).
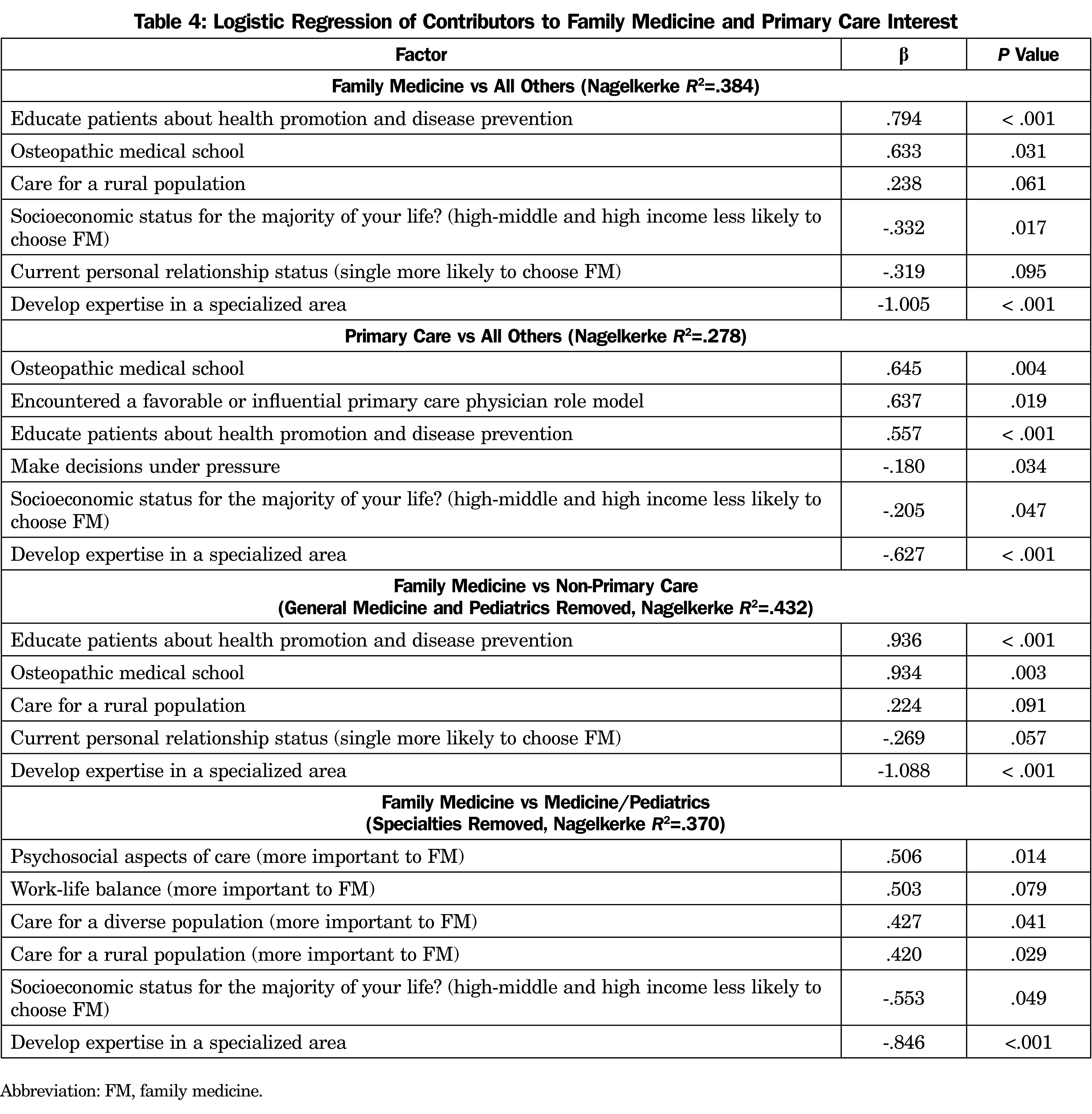
Results of multiple conditional logistic regressions are shown in Table 4. The consistent themes across the analyses were that independent positive predictors of FM and primary care were osteopathic training and the importance of educating patients about health promotion and disease prevention. The common negative predictor was the desire to develop expertise in a specialized area. A desire to care for rural populations was associated with FM, not primary care. Other factors that positively predicted some of the FM/primary care outcomes included growing up in a lower socioeconomic status household (self-classified) and current relationship status (single more likely to choose FM in the regression, but not in the bivariate analysis). We also found differences between FM and internal medicine/pediatrics (other specialties removed).
The PRUS scale was the only physician-centric instrument we used. It has four subparts: general patient care anxiety, fear of bad outcomes, sharing bad outcomes with patients and sharing bad outcomes with other physicians. Comparing scores by primary vs specialty care, there was a difference in worry about bad outcomes (2.02 vs 1.88, P=.020) and share uncertainty with patients subscales (2.36 vs 2.55, P=.012), but not the other two subscales. There were no differences in these subscales between FM and all other respondents, nor between FM and internal medicine/pediatrics with the other specialties removed.
We found that CwU was not associated with either FM career choice or primary care career choice among US medical students by a composite of three commonly used scales, or of those scales individually.
The results of our study could imply that CwU is not important in the work lives of primary care physicians. However, we believe that many lines of evidence tell us this is not the proper conclusion (for all the reasons listed in the Introduction). We can at least conclude in this large cohort of medical students that many other factors were stronger predictors of FM and primary care career choice.
We found differences in two of the PRUS subscales that went in opposite directions. Primary care students were more comfortable sharing their uncertainties with their patients (lower CwU score), but were less comfortable with potential bad outcomes. The absolute magnitude of the differences were small. However, this finding may help explain why we did not find any difference in the overall PRUS score between primary vs specialty care, or FM vs all others.
Some of our results are mostly consistent with previous studies of student career choice when analyzed as bivariate comparisons. Positive predictors for FM or primary care included osteopathic students more likely than allopathic,30 lower household income growing up,31,32 plan to care for diverse and underserved populations,33 and had a primary care role model.34 Negative predictors included opportunities to do research,35,36 the importance of a prestigious career,35 the importance of higher income,34,35, 37-40 and the importance of using advanced technologies.26 Compared to some previous studies, a notable factor that was not associated with FM choice included parents are physicians.41,42 We also found no association with student debt burden and FM and primary care career choice, which is consistent with the majority of the literature.33,34,41,43
On the issue of rurality, our results were different from previous literature. Previous research found that students with a rural background were more likely to choose FM,41,42 but this was not found in our study. Students who said they intended to care for rural populations was a single independent predictor for FM in our logistic regression model, but not primary care. In our cohort, intention for rural training predicted FM choice as a bivariate correlation, but not in the multivariate analysis. Our finding that rural career interest is more associated with FM than other primary care fields was found in another US region as well, suggesting that policy makers aiming to increase rural primary care physician supply should prioritize FM.44
Strengths of our study include prospective design, career results based on match data, not student intent early in their medical school career, and our ability to discern long-term primary care career goals for students who matched in internal medicine or pediatrics.
Our study has limitations. Han et al found that tolerance of ambiguity, but not uncertainty or risk, increased from the first year to fourth year of medical school.29 Perhaps we would have had different results if we studied first-year students. Other studies found that tolerance of ambiguity did (change in both directions depending on baseline tolerance)45 and did not46 change during medical school. Evans found that the third year of medical school may be an opportune time for medical educators to help shape students’ reaction to uncertainty.47 We did not inquire about previous exposure to family medicine outside of the required clerkship, other than their primary care exposure as a patient growing up.
The majority of our students were in Texas medical schools. Other regions might yield different results. The average reported student loan debt was less than national averages, as expected. The average student debt at all RRNeT medical schools in Texas is less than the national average.48 We did not receive information from the medical schools about match results prior to the SOAP process. However, our results did not change when we analyzed them based on career choice in their third years of medical school before the match.
How do we react to these findings? Han, et al have recognized the considerable gaps in our knowledge of what uncertainty is, how it affects people, and how and why it should be communicated.6 Yet ample evidence has shown the many positive effects to physicians, patients, and health care systems using the existing scales to measure CwU and other methods. We used the scales most often used in this literature. There may be aspects of decision making that reflect CwU that are not precisely captured in these scales, such as family physicians’ comfort with formulating diagnoses and plans with their patients without obtaining every possible test they could order.49 Perhaps there is room for another attempt at creating a CwU scale that more purposefully includes concrete decisions in practice such as ordering tests, making diagnoses, and prescribing treatment plans.
CwU may be a teachable and modifiable attitude for medical students and residents. Uncertainty in physicians involves clinical, environmental, and social aspects of care, and CwU dynamically evolves through iterative cycles of forward planning and self-monitoring.50, 51 US family medicine clerkship directors reported that they both teach and demonstrate CwU when dealing with competing clinical guidelines, though they also reported discussing uncertainty was the least-addressed teaching objective.52 Some have called for purposefully teaching CwU in generalist residency training and all physician training—a proposal which we support.3, 53 Models currently exist that support including uncertainty training in residency curricula. Helou, et al developed a framework for understanding medical decision making in the context of uncertainty.54 Randall developed an approach to teaching students about uncertainty starting with the recognition that the realities of clinical medicine are a “disorienting dilemma” for students, which should ultimately transform into an acceptance that they can say, “I don’t know.”55
Implications for Policy
Family medicine residents have recognized CwU as part of their identity, but have also developed tactics to minimize uncertainty.56 In short, we believe that CwU is an important part of the mental makeup of successful and effective family physicians, and is important for positive patient and health care system outcomes. Students who are more comfortable with uncertainty are not currently self-selecting into family medicine or other primary care fields, while it is also true that CwU might be teachable to some degree (or at least role-modeled). This situation is a problem for family medicine.
Future researchers should revisit the concept of CwU in primary care. There may be a discrepancy between the content of existing instruments and family physicians’ concepts of CwU (eg, whether or not to refer to a specialist). Medical educators and national FM organizations may also use our findings to reflect how much they explicitly state that CwU is an important feature of family medicine. Students will have no way of knowing that CwU is important to a family medicine career if no one tells them.
Acknowledgments
Funding Statement: RRNET has support from the Texas Academy of Family Physicians Foundation (TAFP-F), the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant UL1 TR002645. The content is solely the responsibility of the authors and does not necessarily represent the official views of the TAFP-F or National Institutes of Health.
Presentations: A preliminary version of this work was presented at the 2020 NAPCRG Annual Meeting (virtual).
Disclosures: Dr Young discloses that he is the sole owner of Sentire, LLC, which is a novel primary care documentation, coding, and billing system. The other authors have no conflicts to declare. The contents of this article are solely the views of the authors and do not necessarily represent the official views of the Uniformed Services University of the Health Sciences, the US Air Force, or the US Department of Defense.
References
- Salisbury H. Helen Salisbury: risk taking and decision making. BMJ. 2020;368:m573. doi:10.1136/bmj.m573
- McCartney M. Margaret McCartney: why do we ignore uncertainty? BMJ. 2018;360:k1164. doi:10.1136/bmj.k1164
- Simpkin AL, Schwartzstein RM. Tolerating uncertainty - the next medical revolution? N Engl J Med. 2016;375(18):1713-1715. doi:10.1056/NEJMp1606402
- Nevalainen M, Kuikka L, Sjoberg L, Eriksson J, Pitkala K. Tolerance of uncertainty and fears of making mistakes among fifth-year medical students. Fam Med. 2012;44(4):240-246.
- Russek NS, Detsky AS, Quinn KL. Managing clinical uncertainty: a teachable moment. JAMA Intern Med. 2020;180(3):452-453. doi:10.1001/jamainternmed.2019.6700
- Han PKJ, Babrow A, Hillen MA, Gulbrandsen P, Smets EM, Ofstad EH. Uncertainty in health care: towards a more systematic program of research. Patient Educ Couns. 2019;102(10):1756-1766. doi:10.1016/j.pec.2019.06.012
- Gerrity MS, White KP, DeVellis RF, Dittus RS. Physician’s reactions to uncertainty: refining the constructs and scales. Motiv Emot. 1995;19(3):175-191. doi:10.1007/BF02250510
- Beresford EB. Uncertainty and the shaping of medical decisions. Hastings Cent Rep. 1991;21(4):6-11. doi:10.2307/3562993
- Nevalainen MK, Mantyranta T, Pitkala KH. Facing uncertainty as a medical student--a qualitative study of their reflective learning diaries and writings on specific themes during the first clinical year. Patient Educ Couns. 2010;78(2):218-223. doi:10.1016/j.pec.2009.07.011
- Iannello P, Mottini A, Tirelli S, Riva S, Antonietti A. Ambiguity and uncertainty tolerance, need for cognition, and their association with stress. A study among Italian practicing physicians. Med Educ Online. 2017;22(1):1270009. doi:10.1080/10872981.2016.1270009
- Cooke GP, Doust JA, Steele MC. A survey of resilience, burnout, and tolerance of uncertainty in Australian general practice registrars. BMC Med Educ. 2013;13(1):2. doi:10.1186/1472-6920-13-2
- Holt C, Han P, Siewers A, Williams A. Tolerance for uncertainty and risk among academic family medicine practitioners: a CERA survey. Presented at: North American Primary Care Research Group; 2015; Cancun, Mexico.
- Simpkin AL, Vyas JM, Armstrong KA. Diagnostic reasoning: an endangered competency in internal medicine training. Ann Intern Med. 2017;167(7):507-508. doi:10.7326/M17-0163
- Pedersen AF, Carlsen AH, Vedsted P. Association of GPs’ risk attitudes, level of empathy, and burnout status with PSA testing in primary care. Br J Gen Pract. 2015;65(641):e845-e851. doi:10.3399/bjgp15X687649
- Scott AM, Del Mar C. Controlling antibiotic prescribing for lower respiratory tract infections. BMJ. 2017;357:j2398. doi:10.1136/bmj.j2398
- Farnan JM, Johnson JK, Meltzer DO, Humphrey HJ, Arora VM. Resident uncertainty in clinical decision making and impact on patient care: a qualitative study. Qual Saf Health Care. 2008;17(2):122-126. doi:10.1136/qshc.2007.023184
- Ooi K. The Pitfalls of Overtreatment: Why More Care is not Necessarily Beneficial. Asian Bioeth Rev. 2020;12(4):399-417. doi:10.1007/s41649-020-00145-z
- Allison JJ, Kiefe CI, Cook EF, Gerrity MS, Orav EJ, Centor R. The association of physician attitudes about uncertainty and risk taking with resource use in a Medicare HMO. Med Decis Making. 1998;18(3):320-329. doi:10.1177/0272989X9801800310
- O’Riordan M, Dahinden A, Aktürk Z, et al. Dealing with uncertainty in general practice: an essential skill for the general practitioner. Qual Prim Care. 2011;19(3):175-181.
- DeForge BR, Sobal J. Intolerance of ambiguity among family practice residents. Fam Med. 1991;23(6):466-468.
- van der Weijden T, van Bokhoven MA, Dinant GJ, van Hasselt CM, Grol RP. Understanding laboratory testing in diagnostic uncertainty: a qualitative study in general practice. Br J Gen Pract. 2002;52(485):974-980.
- Donner-Banzhoff N. [Dealing with uncertainty in general medical practice]. Z Evid Fortbild Qual Gesundhwes. 2008;102(1):13-8. Umgang mit Unsicherheit in der Allgemeinmedizin. doi:10.1016/j.zgesun.2007.12.001
- Gordon GH, Joos SK, Byrne J. Physician expressions of uncertainty during patient encounters. Patient Educ Couns. 2000;40(1):59-65. doi:10.1016/S0738-3991(99)00069-5
- DeForge BR, Sobal J. Intolerance of ambiguity in students entering medical school. Soc Sci Med. 1989;28(8):869-874. doi:10.1016/0277-9536(89)90117-2
- Morgan M, Jenkins L, Ridsdale L. Patient pressure for referral for headache: a qualitative study of GPs’ referral behaviour. Br J Gen Pract. 2007;57(534):29-35.
- Merrill JM, Lorimor RJ, Thornby JI, Vallbona C. Reliance on high technology among senior medical students. Am J Med Sci. 1998;315(1):35-39. doi:10.1097/00000441-199801000-00007
- Gerrity MS, DeVellis RF, Earp JA. Physicians’ reactions to uncertainty in patient care. A new measure and new insights. Med Care. 1990;28(8):724-736. doi:10.1097/00005650-199008000-00005
- Roets A, Van Hiel A. Item selection and validation of a brief, 15-item version of the need for closure scale. Pers Individ Dif. 2011;50(1):90-94. doi:10.1016/j.paid.2010.09.004
- Han PK, Schupack D, Daggett S, Holt CT, Strout TD. Temporal changes in tolerance of uncertainty among medical students: insights from an exploratory study. Med Educ Online. 2015;20:28285. eCollection 2015. doi:10.3402/meo.v20.28285
- Phillips JP, Wendling A, Bentley A, Marsee R, Morley CP. Trends in US medical school contributions to the family physician workforce: 2018 update from the American Academy of Family Physicians. Fam Med. 2019;51(3):241-250. doi:10.22454/FamMed.2019.395617
- Colquitt WL, Zeh MC, Killian CD, Cultice JM. Effect of debt on U.S. medical school graduates’ preferences for family medicine, general internal medicine, and general pediatrics. Acad Med. 1996;71(4):399-411. doi:10.1097/00001888-199604000-00023
- Kassebaum DG, Szenas PL, Schuchert MK. Determinants of the generalist career intentions of 1995 graduating medical students. Acad Med. 1996;71(2):198-209. doi:10.1097/00001888-199602000-00030
- Senf JH, Campos-Outcalt D, Kutob R. Factors related to the choice of family medicine: a reassessment and literature review. J Am Board Fam Pract. 2003;16(6):502-512. doi:10.3122/jabfm.16.6.502
- Phillips RL, Dodoo M, Petterson SM, et al. What Influences Medical Student & Resident Choices? Robert Graham Center. May 18, 2009. Accessed May 18, 2009. http://www.josiahmacyfoundation.org/documents/pub_grahamcenterstudy.pdf
- Bowman MA, Haynes RA, Rivo ML, Killian CD, Davis PH. Characteristics of medical students by level of interest in family practice. Fam Med. 1996;28(10):713-719.
- Senf JH, Campos-Outcalt D, Kutob R. Family medicine specialty choice and interest in research. Fam Med. 2005;37(4):265-270.
- Kruse J. Income ratio and medical student specialty choice: the primary importance of the ratio of mean primary care physician income to mean consulting specialist income. Fam Med. 2013;45(4):281-283.
- Rosenthal MP, Diamond JJ, Rabinowitz HK, et al. Influence of income, hours worked, and loan repayment on medical students’ decision to pursue a primary care career. JAMA. 1994;271(12):914-917. doi:10.1001/jama.1994.03510360040033
- Lewis CE, Prout DM, Chalmers EP, Leake B. How satisfying is the practice of internal medicine? A national survey. Ann Intern Med. 1991;114(1):1-5. doi:10.7326/0003-4819-114-1-1
- Ebell MH. Future Salary and US Residency Fill Rate Revisited. JAMA.2008;300(10):1131–1132. doi:10.1001/jama.300.10.1131
- Bland CJ, Meurer LN, Maldonado G. Determinants of primary care specialty choice: a non-statistical meta-analysis of the literature. Acad Med. 1995;70(7):620-641. doi:10.1097/00001888-199507000-00013
- Meurer LN. Influence of medical school curriculum on primary care specialty choice: analysis and synthesis of the literature. Acad Med. 1995;70(5):388-397. doi:10.1097/00001888-199505000-00015
- Phillips JP, Weismantel DP, Gold KJ, Schwenk TL. Medical student debt and primary care specialty intentions. Fam Med. 2010;42(9):616-622.
- Wendling AL, Short A, Hetzel F, Phillips JP, Short W. Trends in Subspecialization: A Comparative Analysis of Rural and Urban Clinical Education. Fam Med. 2020;52(5):332-338. doi:10.22454/FamMed.2020.182557
- Geller G, Grbic D, Andolsek KM, Caulfield M, Roskovensky L. Tolerance for ambiguity among medical students: patterns of change during medical school and their implications for professional development. Acad Med. 2020. doi:10.1097/ACM.0000000000003820
- Geller G, Faden RR, Levine DM. Tolerance for ambiguity among medical students: implications for their selection, training and practice. Soc Sci Med. 1990;31(5):619-624. doi:10.1016/0277-9536(90)90098-D
- Evans L, Trotter DR, Jones BG, et al. Epistemology and uncertainty: a follow-up study with third-year medical students. Fam Med. 2012;44(1):14-21.
- Which medical graduates have the most debt? US News & World Report. Accessed Oct 18, 2021. https://www.usnews.com/best-graduate-schools/top-medical-schools/debt-residents-rankings
- Young RA, Bayles B, Benold TB, Hill JH, Kumar KA, Burge S. Family physicians’ perceptions on how they deliver cost-effective care: a qualitative study from the Residency Research Network of Texas (RRNeT). Fam Med. 2013;45(5):311-318.
- Ilgen JS, Bowen JL, de Bruin A, Regehr G, Teunissen PW. “I Was Worried About the Patient, but I Wasn’t Feeling Worried”: How Physicians Judge Their Comfort in Settings of Uncertainty, Academic Medicine: November 2020 - Volume 95 - Issue 11S - p S67-S72. doi:10.1097/ACM.0000000000003634
- Ilgen JS, Eva KW, de Bruin A, Cook DA, Regehr G. Comfort with uncertainty: reframing our conceptions of how clinicians navigate complex clinical situations. Adv Health Sci Educ Theory Pract. 2019;24(4):797-809. doi:10.1007/s10459-018-9859-5
- Ledford CJ, Seehusen DA, Chessman AW, Shokar NK. How we teach U.S. medical students to negotiate uncertainty in clinical care: a CERA study. Fam Med. 2015;47(1):31-36.
- Hoffman JR, Kanzaria HK. Intolerance of error and culture of blame drive medical excess. BMJ. 2014;349(oct14 3):g5702. doi:10.1136/bmj.g5702
- Helou MA, DiazGranados D, Ryan MS, Cyrus JW. Uncertainty in decision making in medicine: a scoping review and thematic analysis of conceptual models. Acad Med. 2020;95(1):157-165. doi:10.1097/ACM.0000000000002902
- Randall V, Villareal C. It’s okay to say ‘I don’t know’": medical students use transformative thinking to cope with ambiguity and uncertainty. MedEdPublish. 2020. doi:10.15694/mep.2020.000014.1
- Ledford CJ, Cafferty LA, Seehusen DA. Socializing identity through practice: a mixed methods approach to family medicine resident perspectives on uncertainty. Fam Med. 2015;47(7):549-553.