Background and Objective: In 2014, the Accreditation Council for Graduate Medical Education (ACGME) implemented numeric requirements for family medicine (FM) pediatric patient encounters. Impact on residency programs is unclear. We aimed to identify any difficulties faced by FM program directors (PDs) meeting these numeric requirements.
Methods: Questions about pediatric training in family medicine residencies were included in a survey of PDs conducted by the Council of Academic Family Medicine Educational Research Alliance (CERA). We performed univariate analysis of the demographic and program characteristics. We then used χ2 tests of independence to test for bivariate associations between these characteristics and our primary outcome: the most difficult ACGME pediatric care requirement to meet.
Results: Most programs reported the hospital as the primary location of training (n=131, 46%) and their family medicine practice (FMP) patient population consisted of over 20% pediatric patients (n=153, 56%). Over 80% of program directors reported challenges meeting FM requirements for the care of children. Challenges meeting pediatric requirements were associated with fewer than 20% FMP patients under 19 years of age (P<.0001), fewer than 50% of core FM faculty caring for sick children (P=.0128), and primary location of pediatric training in a family health center (P=.0006).
Conclusion: Difficulty meeting ACGME requirements for the care of children in FM residency programs is common, especially for programs with fewer than 20% FMP patients under 19 years of age. Further research is needed to determine how best to assure FM resident competencies in the care of children and adolescents.
Family physicians play a crucial role in the delivery of care for children, especially in rural locations and areas with low pediatrician density. 1, 2 Historically, family physicians provide about 20% of pediatric visits nationally.3 Family medicine (FM) department chairs endorse modeling full-scope family medicine as an important way to encourage graduates practicing full-scope family medicine, which includes pediatric care. 4
Despite the important role family physicians play in the care of children, the number who care for children, especially sick children in hospitals, has decreased steadily over the past few decades. 2, 5 Between 2014 and 2018, the proportion of family physicians providing continuity care of young children under the age of 5 years declined from 92.5% to 87%, and for older children aged 5-18 years from 76.4% to 69.4%. 6 Among FM graduates in 2016, while 86% were providing pediatric outpatient care, only 20% were practicing inpatient pediatrics, and fewer than 30% were providing newborn hospital care 3 years postgraduation. 7 A study in Vermont demonstrated the odds of children attending a family medicine practice were 5% less over time. 8
The reasons for the decline in family physicians providing pediatric care are unclear. Increased competition from pediatric practices, increased number of pediatricians, falling birth rates, decline in family physicians providing obstetric services, lack of child-friendly waiting rooms and services, costs associated with vaccines, inadequate training in residency, relocation of emergency and hospital services to tertiary care centers, loss of hospital privileges in nursery and inpatient units, concerns about insurance reimbursement, and media representation and public perception have all been hypothesized to contribute. 9-11 Despite this decline, on average, the care of children still encompasses 10% of family physicians’ practice time. 3 Resident training impacts future practice, but there is scant information on pediatric training in FM residency programs; the last published study documenting pediatric training time was in 1992. 11 In 2016, FM residency graduates largely reported feeling “adequately prepared” by their programs to provide pediatric care in outpatient (92%) settings, but less so in inpatient settings (76%). 7
The ACGME implemented program requirements in 2014 that included changes regarding the quantity of pediatric patient encounters; these modifications remain a part of the 2022 guidelines. 12 These guidelines require at least 200 hours (or 2 months) and 250 patient encounters dedicated to the care of ill child patients in the hospital and/or emergency setting. 12 It is not clear how these requirement changes impacted residency programs. The primary objective of our study was to understand the current state of pediatric training in FM residency programs as reported by the PDs, including factors of amount of time, location of training, faculty, and investigate how these characteristics relate to challenges meeting ACGME requirements.
Survey Mechanism and Instrument
The pediatric training questions developed for this study were part of a larger omnibus survey conducted by the Council of Academic Family Medicine Educational Research Alliance (CERA). The methodology of the CERA Program Director Survey has previously been described in detail. 13 The project was approved by the American Academy of Family Physicians Institutional Review Board in September 2020. Data were collected from September 23 to October 16, 2020.
The survey was emailed to 664 program directors (PDs) and contained a qualifying question to remove programs that had not had three resident classes; 40 PDs who did not meet criteria were removed from the sample, reducing the sample size to 624. The overall response rate for the survey was 50.00% (312/624) but because questions were not required to be answered, response rates for each question vary and 29 PDs only completed the demographic questions, leaving an analyzable sample size of 283 (45%).
In addition to program demographic data, we gathered curricular and faculty data related to pediatric training. Demographic characteristics included program type (university, community, military), location divided by region of the United States, community size, and number of residents in the program. Curricular and faculty characteristics included presence of a pediatrics residency in the same institution, number of months or blocks of time devoted to pediatrics, presence of pediatrician as a member of residency core faculty, the percent of patients in the FMP under the age of 19, and percentage of FM faculty members who provide hospital care for newborns or pediatric inpatients. We inquired about location of training in pediatrics, offering choices of a variety of settings. In addition, PDs were asked to indicate the area in which they had the most difficulty meeting ACGME requirements for number of encounters, with choices including FMP visits for children under 10 years; ill child encounters in the hospital or emergency department (ED); ED encounters; inpatient encounters; pediatric ambulatory visits; newborn encounters; or none of the above. PDs could choose only one option.
Data Analysis
Respondents to the survey indicated the United States Census Division in which their program was located, which we then recategorized into the four Census Regions. Questions with a numeric response including number of residents, pediatric patient percentage, number of pediatric blocks, and percentage of faculty caring for sick children or newborns in hospital were categorized based on natural breaking points in the response distribution.
We performed univariate analysis of the demographic and program characteristics. We then used χ2 tests of independence to test for bivariate associations between these characteristics and the hardest ACGME pediatric care requirement to meet. Due to sample size limitations, some levels were combined, and others were omitted when performing the tests. We performed false discovery rate adjustment to account for multiple testing while maintaining more statistical power than with comparable adjustment methods. 14 We conducted all analyses using SAS software version 9.4 (SAS Institute, Cary, NC).
Program Characteristics
Table 1 includes demographic descriptions of the responding FM residency programs. Overall, 60% (n=170) of the 283 programs included in our analyses were community based but university affiliated. Responding programs represented all four areas of the country and all community sizes ranging from rural to urban. Compared to the entire CERA data set of programs, responding programs were significantly less likely to be located in the Midwest (17% vs 24%) or Pacific (13% vs 17%) regions (P=.01). A majority (85%, n=239) of the programs reported fewer than 31 total residents.
|
|
n (%)
|
|
Total
|
|
283
|
|
Type of program
|
University based
Community based, university affiliated
Community based, nonaffiliated
Military
|
45 (15.9)
170 (60.1)
63 (22.3)
5 (1.8)
|
|
Location*
|
Northeast
Midwest
South
West
|
58 (20.5)
76 (26.9)
87 (30.7)
62 (21.9)
|
|
Community size
|
Less than 30,000
30,000 to 74,999
75,000 to 149,000
150,000 to 499,999
500,000 to 1 million
More than 1 million
|
30 (10.6)
52 (18.4)
55 (19.5)
68 (24.1)
35 (12.4)
42 (14.9)
|
|
Total resident number
|
<19
19-31
>31
|
108 (38.3)
131 (46.5)
43 (15.2)
|
Pediatric training characteristics are summarized in Table 2. Programs in the same institution as a pediatric residency made up 33% (n=94) of our sample. Forty-one percent of programs had less than 5 dedicated pediatric months or blocks (n=115) while 59% had 5 or more blocks (n=165). PDs reported a median of 20% of patients in FMP under the age of 19 years, with 44% of programs reporting less than 20% (Table 2). Core FM faculty had variable participation in the care of newborns or sick children in the hospital. The median percent of core faculty in each program that cares for newborns in the hospital was 60% while the median that cares for sick children was 25%. A total of 32% (n=89) of programs reported 100% faculty participation in newborn care and 27% (n=75) reported 100% faculty participation in inpatient sick-child care.
|
|
n (%)
|
|
Total
|
|
283
|
|
Percent of family health center patients under 19 years old
|
<20
20+
|
120 (44.0)
153 (56.0)
|
|
Pediatric residency within institution
|
Yes
No
|
94 (33.5)
187 (66.5)
|
|
Dedicated pediatric months/blocks
|
<5
5+
|
115 (41.1)
165 (58.9)
|
|
Pediatrician as part of core faculty
|
Yes
No
|
61 (21.6)
222 (78.4)
|
|
Percent of family medicine faculty who care for newborns in hospital
|
0
1-49
50-99
100
|
53 (18.9)
68 (24.2)
71 (25.3)
89 (31.7)
|
|
Percent of family medicine faculty who care for sick children in hospital
|
0
1-49
50-99
100
|
106 (37.7)
49 (17.4)
51 (18.1)
75 (26.7)
|
Setting of Pediatric Training
Table 3 highlights the setting where most pediatric training occurs for FM residents. In most (46%, n=131) programs, pediatric training was hospital based, while 19% (n=54) of PDs indicated most pediatric training occurred in an outpatient setting. Many (32%, n=90) reported an even division between a combination of settings. Most of the 131 hospital-based locations were in tertiary care facilities (59%, n=77) and the rest in community hospital settings (41%, n=54). There was no difference in use of a tertiary children’s hospital by region (P=.65). Of the 54 programs reporting a primary outpatient setting, most (63%, n=34) reported the FMP as the primary site.
|
Training Location
|
n (%)
|
|
Total
|
283
|
|
Primary Hospital
|
131 (46.3)
|
|
Community hospital
|
54 (19.1)
|
|
Free- standing children’s hospital
|
47 (16.6)
|
|
Children’s unit within a tertiary care or university teaching hospital
|
30 (10.6)
|
|
Primary Outpatient
|
54 (19.1)
|
|
Family health center/family medicine practice
|
34 (12.0)
|
|
External pediatric practice
|
20 (7.1)
|
|
Multiple Locations
|
90 (31.8)
|
|
Equally between a community and children-specific site
|
40 (14.1)
|
|
Equally between a university teaching hospital and family practice center
|
27 (9.5)
|
|
Equally in all of the above
|
23 (8.1)
|
|
Other
|
8 (2.8)
|
Challenges Meeting Requirements
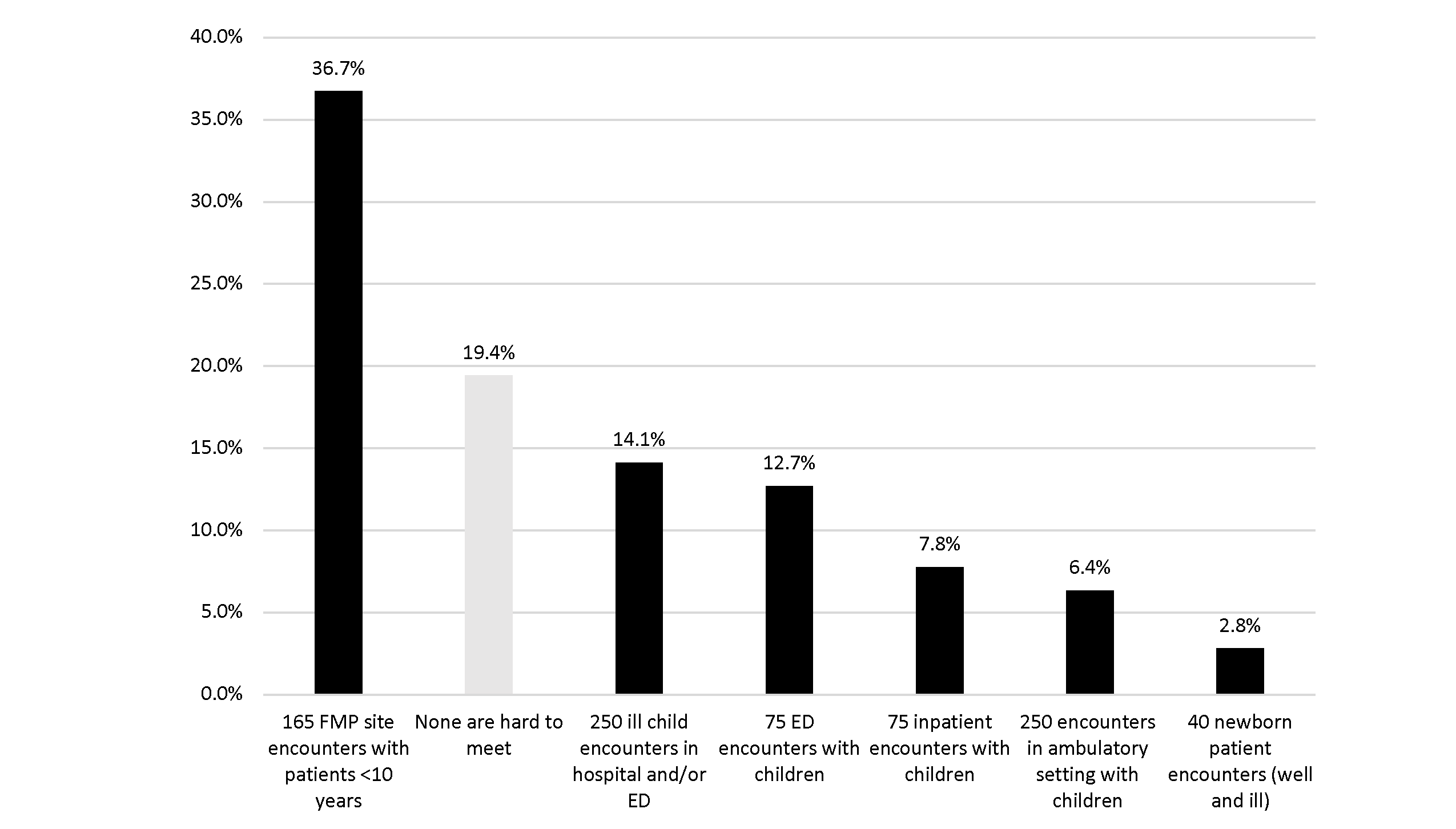
Only 19% (n=55) of PDs reported no challenges meeting the ACGME requirements for the care of children (Figure 1). The most commonly-reported challenge was meeting adequate numbers of pediatric patients under the age of 10 years in the FMP (37%, n=104), followed by completing 250 encounters with sick children in the hospital (inpatient or ED; 14%, n=40). Completion of 40 newborn patient encounters was the requirement least likely to pose difficulty (2.8%, n=8).
When analyzing areas of difficulty by demographic and program characteristics (Appendix Table A), the only characteristics that demonstrated a significant association with meeting requirements were the percent of patients under the age of 19 years in the FMP (P<.0001), the location of the majority of training (P=.0006), and the percentage of core faculty who care for sick children inpatient (P=.0128). Programs with more than 20% of their patients under the age of 19 years in the FMP had less difficulty meeting the requirement for 165 visits in the FMP and made up a higher percentage of the 55 programs reporting no difficulties (81.8%, n=45). Those programs utilizing multiple sites as opposed to one primary site of pediatric training made up 40% (n=22) of the 55 programs that reported no difficulties. Other models fared worse, with those reporting no difficulties ranging from 0% (n=0) for those concentrated in an external pediatric practice, to 20% (n=11) for those concentrated in a freestanding children’s hospital.
We found no statistically significant differences in requirements that were hard to meet in terms of program type (P=.1703), program region (P=.4142), community size (P=.4142), number of residents (P=.6917), presence of a pediatric residency within the same institution (P=.4142), over or under 5 blocks of pediatric trainings (0.4142), presence of a pediatrician on core faculty (P=.6917), or percent of core faculty caring for newborns (P=.1072). However, there was an insignificant trend between a community size of over 1 million and the ability to meet requirements: 38% of respondent programs in communities over 1 million do not find any requirements hard to meet, compared to 19% on average and only 12% to 13% in communities of fewer than 75,000.
More than 80% of PDs report challenges in meeting at least one ACGME requirement in our sample. While most programs offer at least 5 months/blocks of dedicated training, the biggest challenge reported was meeting adequate numbers of encounters with children under 10 years of age in the FMP. Additionally, almost half (44%) of respondents reported that fewer than 20% of their FMP population are children, and this factor was significantly associated with program difficulty meeting numbers. FM programs will need to focus on increasing pediatric ambulatory volume to meet AGME requirements. Recent data demonstrating that family physicians working in academic settings see more children under the age of 5 years than those in different practice settings, but that the same does not hold for older children, suggests that there may be a great deal of complexity around when and how pediatric patients enter care at an FMP. 2 As Page et al described in their experience in North Carolina, 15 programs may need to embark on a concentrated quality improvement effort to increase pediatric volumes and competencies.
The total amount of time residents focus on pediatrics has remained relatively stable since the 1990s, with most programs dedicating 5 blocks to pediatric-specific rotations, most of which occur in hospital-based settings. Despite the stability of time spent in pediatric education over time and the location, the second-biggest challenge noted by PDs was meeting the ACGME requirements for caring for sick children, with 35% of PDs reporting a challenge in the inpatient unit, ED, or both. These results suggest that total the factors of time spent and location are not sufficient measures. We believe this might be due to a larger shift toward ambulatory management and away from hospital-based management of many pediatric conditions, as pediatric hospitalizations have been steadily falling for decades. 14 Our data suggest that focusing on pediatric patient population in the FMP, assuring adequate volume of sick children in hospital settings, and faculty skill set may be higher yield than focusing on blocks or time spent in dedicated rotations.
Little is known about the ideal location for pediatric education; one Canadian study demonstrated similar resident satisfaction and confidence when comparing those in an all-outpatient rotation to those with a combined inpatient-outpatient rotation, and potentially superior knowledge acquisition in a focused pediatric outpatient specialty model. 16 Interestingly, only 6% of respondents indicated challenges with meeting numbers for ambulatory encounters, which raises the question of where these encounters may be happening, if not the FMP. With 7% indicating a pediatric practice as a site of majority of training, and multiple responses indicating a combination of sites, it seems likely that some of these ambulatory numbers are coming from external clinics. Based on the data from this study, assuring adequate volume by using multiple sites may be an effective approach to meeting the ACGME requirements for volume.
For the hospital-based portion of a curriculum, we know that most FM programs are community based and many rely on community hospital volume for care, 17 which our data support. There has been a significant trend in pediatrics toward consolidating care in children’s hospitals. 18 We found that 27% of FM residency programs in our sample rely on these hospitals or tertiary care centers for the majority or some resident training in pediatrics. The recent pandemic has accelerated the drop in pediatric inpatient volumes with fewer children becoming sick, 19 making it likely that challenges will have increased in the last 2 years for the hospital-based components (ED, inpatient).
The variability and overall small number of FM core faculty who care for sick children in the hospital may have long-term implications for the number of family physicians who care for children. As noted by Backer in 2005, FM residency programs have a key role to play in better equipping family physicians to take care of children and need to stress the care of hospitalized patients. 10 It seems possible that increasing the number of family physicians on residency faculties who include inpatient pediatric work in their practice could help to improve this situation. As Peterson et al reported in 2015, 4 FM chairs strongly believe that modeling full-scope family medicine will lead to graduates practicing full-scope family medicine, which includes pediatric care. With more than one-third of programs reporting no FM faculty care for sick children in a hospital setting, many programs are not modeling this competency for their residents.
It is important to highlight what our study did not find. We found no statistically significant associations when comparing difficulty meeting requirements with region of the country or community size, which is perhaps surprising given that region and rurality are associated with ongoing care of children by practicing family physicians according to ABFM data. 2 Over 86% of programs in communities smaller than 75,000 reported a challenge meeting requirements while only 62% in communities over 1 million reported a challenge, implying that there may be an association despite our inability to detect a difference given our limited statistical power. Additionally, the number of residents in a program did not make a difference, nor did the number of rotations, but we cannot assess the content and context of these experiences and cannot make an accurate assessment of how much time is adequate to obtain competency. FM programs’ ability to meet pediatric encounter requirements are not significantly impacted by having a pediatric residency program within the same institution. Further research will need to delve into the factors that allow for FM residency programs to be successful in training residents to care for children.
Future Directions
The reason for the reduction in pediatric care by family physicians in the United States over the past 2 decades is unclear, and likely multifactorial. Further research is needed to better understand the link between residency training models and the outcome of caring for children in practice. Additionally, the role of who is teaching and role modeling needs further investigation. With few FM faculty providing hospital care and many residents being sent to tertiary care children’s hospitals, future research will need to explore the risks and benefits of this approach.
Finally, further investigation is needed to understand factors that improve resident likelihood to provide pediatric care after graduation and factors that affect residency faculty engaging in inpatient and nursery care. Future studies can evaluate the relationship between where and how family medicine residents are trained and whether they end up caring for children in practice.
Limitations
Our study is limited by the use of a cross-sectional survey with a less than 50% response rate and an undersampling of the Midwest and Pacific regions. We cannot be certain that the responses are reflective of all FM programs. Additionally, given the limited number of questions and potential for ambiguity in responses, it is possible that some questions may have been interpreted in a way that is not reflective of what is happening in an individual institution. Finally, some responses were limited by sample size, limiting the ability to adequately put all variables into the statistical modeling and having to consolidate some variables.
Having difficulty meeting ACGME requirements for the care of children in FM residency programs is common and is associated with the location of most pediatric training, the number of patients under the age of 19 years in the FMP, and the percentage of faculty who provide inpatient care to children. Therefore, improvements in the ability to meet requirements will be more challenging than merely adding months into curricula, as months alone are not associated with any difference in a program’s reported level of difficulty in meeting requirements. Such improvement will require an approach that addresses clinic population, faculty competencies, and details of rotational experiences.
References
-
Makaroff LA, Xierali IM, Petterson SM, Shipman SA, Puffer JC, Bazemore AW. Factors influencing family physicians’ contribution to the child health care workforce. Ann Fam Med
. 2014;12(5):427-431. doi:10.1370/afm.1689
-
Jetty A, Romano MJ, Jabbarpour Y, Petterson S, Bazemore A. A cross-sectional study of factors associated with pediatric scope of care in family medicine. J Am Board Fam Med
. 2021;34(1):196-207. doi:10.3122/jabfm.2021.01.200300
-
Phillips RL Jr, Bazemore AW, Dodoo MS, Shipman SA, Green LA. Family physicians in the child health care workforce: opportunities for collaboration in improving the health of children. Pediatrics
. 2006;118(3):1200-1206. doi:10.1542/peds.2006-0051
-
Peterson LE, Blackburn B, Phillips RL Jr, Mainous AG III. Family medicine department chairs’ opinions regarding scope of practice. Acad Med
. 2015;90(12):1691-1697. doi:10.1097/ACM.0000000000000774
-
Bazemore AW, Makaroff LA, Puffer JC, et al. Declining numbers of family physicians are caring for children. J Am Board Fam Med
. 2012;25(2):139-140. doi:10.3122/jabfm.2012.02.110203
-
Eden AR, Morgan ZJ, Jetty A, Peterson LE. Proportion of family physicians caring for children is declining. J Am Board Fam Med
. 2020;33(6):830-831. doi:10.3122/jabfm.2020.06.200089
-
Peterson LE, Fang B, Puffer JC, Bazemore AW. Wide gap of preparation and scope of practice of early career family physicians. J Am Board Fam Med
. 2018;31(2):181-182. doi:10.3122/jabfm.2018.02.170359
-
Wasserman RC, Varni SE, Hollander MC, Harder VS. Change in site of children’s primary care: a longitudinal population-based analysis. Ann Fam Med
. 2019;17(5):390-395. doi:10.1370/afm.2416
-
Anim TE. The dilution of family medicine: waning numbers of family physicians providing pediatric care.
J Am Board Fam Med. 2020;33(6):828-829.
doi:10.3122/jabfm.2020.06.200544
-
Backer LA. Caring for children: re-examining the family physician’s role. Fam Pract Manag. 2005;12(7):45-52.
-
Baldor RA, Luckmann R. A survey of formal training in the care of children in family practice residency programs. Fam Med. 1992;24(6):426-430.
-
-
Seehusen DA, Mainous AG 3rd, Chessman AW. Creating a centralized infrastructure to facilitate medical education research. Ann Fam Med
. 2018;16(3):257-260. doi:10.1370/afm.2228
-
Krugman SD, Rauch DA. The future of inpatient community hospital care: is there one?
Hosp Pediatr. 2021;11(4):422-426.
doi:10.1542/hpeds.2020-003905
-
Page C, Carlough MC, Lam Y, Steiner J. Reinvigorating pediatric care in an academic family medicine practice. Fam Med. 2014;46(2):120-123.
-
Duke P, Curran V, Hollett A. Training family medicine residents to care for children: what is the best approach? Can Fam Physician. 2011;57(2):e46-e50.
-
Mainous AG 3rd, Seehusen D, Shokar N. CAFM Educational Research Alliance (CERA) 2011 Residency Director survey: background, methods, and respondent characteristics. Fam Med. 2012;44(10):691-693.
-
França UL, McManus ML. Trends in regionalization of hospital care for common pediatric conditions. Pediatrics
. 2018;141(1):20171940. doi:10.1542/peds.2017-1940
-
Chaiyachati BH, Agawu A, Zorc JJ, Balamuth F. Trends in pediatric emergency department utilization after institution of Coronavirus Disease-19 mandatory social. J Pediatr
. 2020;226:274-277.e1. doi:10.1016/j.jpeds.2020.07.048