Background and Objectives: Sparse research exists on evaluating the effects of medical scribing programs on the educational trajectory of prehealth students. This study assesses the impact of the Stanford Medical Scribe Fellowship (COMET) on its prehealth participants’ educational goals, preparation for graduate training, and acceptance into health professional schools.
Methods: We distributed a 31-question survey with both closed- and open-ended questions to 96 alumni. The survey collected participant demographics, self-reported underrepresented in medicine (URM) status, pre-COMET clinical experiences and educational goals, application to and acceptance at health professional schools, and perceived impact of COMET on their educational trajectory. SPSS was used to complete the analyses.
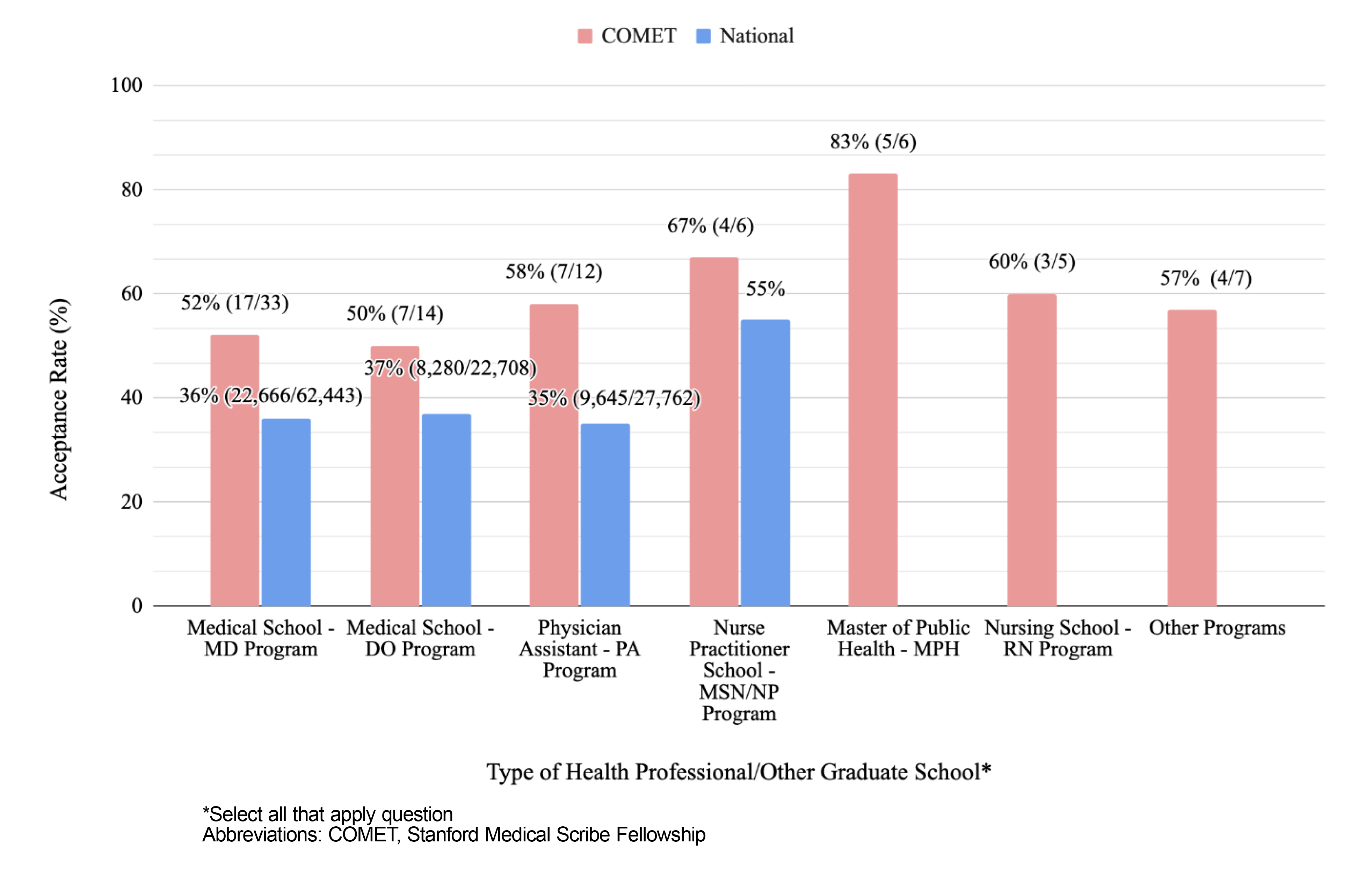
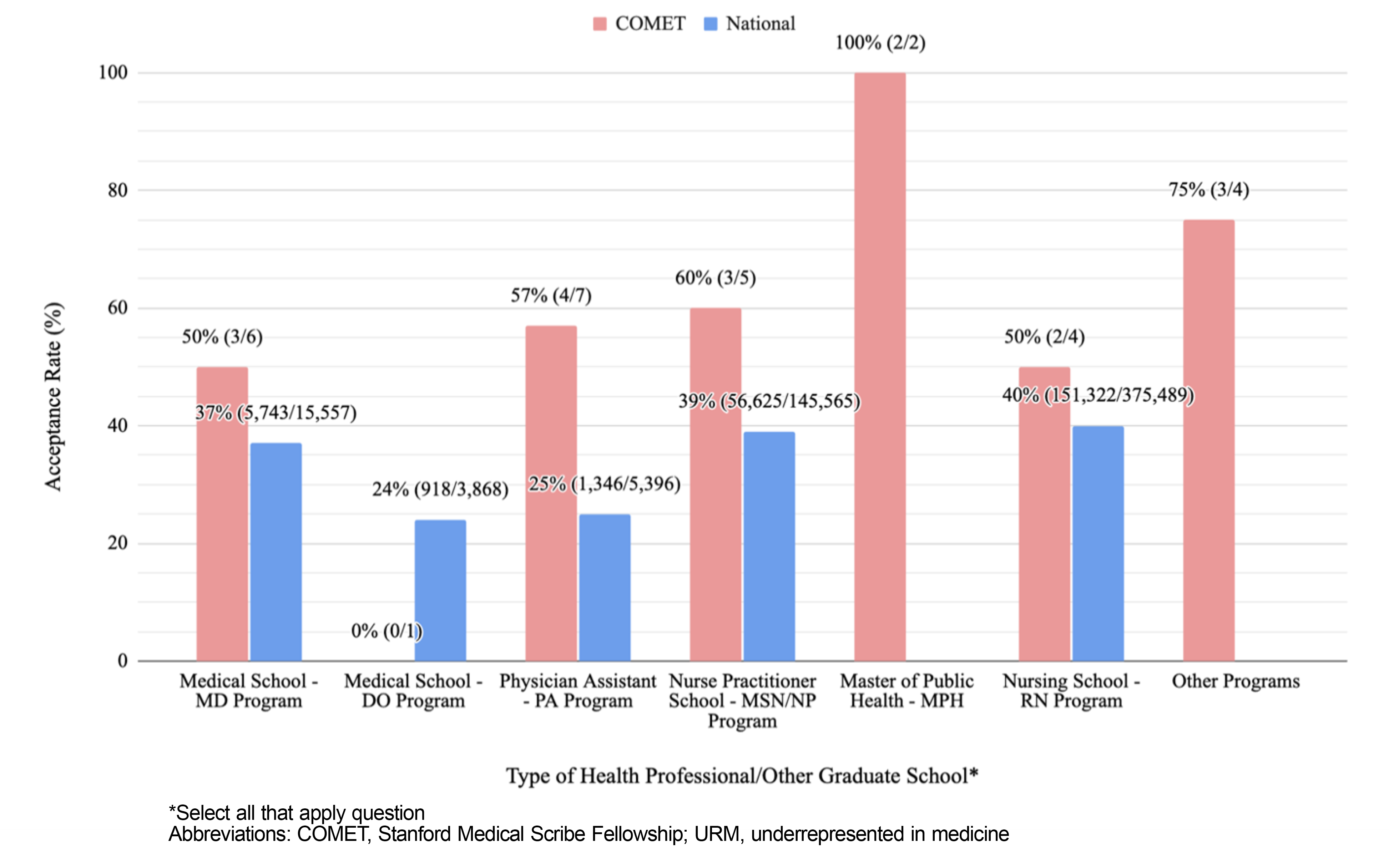
Results: The survey had a 97% (93/96) completion rate. Among all respondents, 69% (64/93) applied to a health professional school and 70% (45/64) were accepted. Among URM respondents, 68% (23/34) applied to a health professional school and 70% (16/23) were accepted. Overall acceptance rates for MD/DO and PA/NP programs were 51% (24/47) and 61% (11/18), respectively. URM acceptance rates for MD/DO and PA/NP programs were 43% (3/7) and 58% (7/12), respectively. For current or recently graduated health professional school respondents, 97% (37/38) “strongly agreed” or “agreed” that COMET helped them succeed in their training.
Conclusions: COMET is associated with a positive impact on the educational trajectory of its prehealth participants and a higher acceptance rate into health professional schools than the national rates for both overall and URM applicants. Scribing programs may serve as pipeline development and help increase the diversity of the future health care workforce.
Medical scribing, in addition to enhancing patient-provider interactions and reducing electronic health record (EHR) clerical burden for clinicians, 1-4 offers a unique educational opportunity for prehealth students to gain clinical immersion, acquire medical knowledge, and practice critical thinking. 5 Many prehealth students choose to work as medical scribes to gain clinical experience, 6 and admissions committees view medical scribing favorably in students’ applications to health professional programs. 7
In recent years, development of postbaccalaureate medical scribing programs has allowed interested prehealth students to connect with clinicians seeking documentation support. 8, 9 Researchers have associated postbaccalaureate premedical programs with an increased likelihood for their participants to practice in underserved areas. 10 By recruiting diverse participants, especially individuals who have faced challenges in applying to health professional schools, 11, 12 postbaccalaureate medical scribing programs may have the potential to increase underrepresented in medicine (URM) matriculation rates.
The Stanford Medical Scribe Fellowship (COMET) is a 1-year postbaccalaureate premedical program, supported by student tuition, that combines an apprenticeship-like scribing experience with teaching, advising, application support, and mentored scholarship. 13 In a previously published 5-year evaluation (where the educational trajectory of graduates was not specifically addressed), research findings associated COMET with high levels of satisfaction among learners and faculty, better preparation for professional schooling among learners, and improved joy of practice among faculty. 8 This follow-up study assesses the impact of COMET on its prehealth participants’ educational goals, preparation for graduate training, and acceptance into health professional schools.
Study Design
We distributed a 31-question survey with both closed and open-ended questions to all COMET alumni from 2015 to 2021. Through the survey, we collected participant demographics, pre-COMET clinical experiences, scholarly work participation during COMET, self-reported application to and acceptance at a health professional school, and perceived impact of COMET on respondents’ educational trajectory.
We calculated MD, DO, and PA program acceptance rates and then researched national acceptance/matriculation rates using publicly available databases 14-18 for comparison for both overall and URM learners. National NP/MSN acceptance/matriculation rates were not available; for comparison, we approximated the national rate by calculating data from the U.S. News & World Report’s “2023 Best Nursing Schools: Master’s Program.” 19 We averaged the acceptance rate data from the top 50 ranked schools in this report. We derived URM-specific NP/MSN and RN program data from a published national survey. 20 No national data were available for MPH programs.
Data Analysis
We used descriptive analyses to examine closed-ended data; we examined open-ended data using deductive content analysis. 21 We used statistical analyses, including the Pearson χ2 test, logistic regression model, and Mann-Whitney U test, to examine the associations between participant demographics and responses with self-reported acceptance at a health professional school. We used IBM SPSS Statistics for Windows, Version 28, to complete the analyses.
Ethical Approval
The Stanford University Institutional Review Board exempted this study from review.
The survey had a 97% (93/96) completion rate. Table 1 shows a detailed breakdown of participant data. Respondents were racially/ethnically diverse; 37% (34/93) identified as URM. Before COMET, many participants had prior clinical experience in shadowing, clinical volunteering, and research. Respondents reported their desired career paths at their time of enrollment in COMET: 66% (61/93) planned on MD, 28% (26/93) on DO, 27% (25/93) on PA, and 9% (8/93) on NP. Ninety-one percent (85/93) of all respondents reported plans to apply to at least one type of health professional or other graduate school prior to starting COMET.
|
Fellowship cohort year
|
Count
|
Percent
|
|
2015-2016
|
2
|
-
|
|
2016-2017
|
5
|
-
|
|
2017-2018
|
10
|
-
|
|
2018-2019
|
16
|
-
|
|
2019-2020
|
28
|
-
|
|
2020-2021
|
32
|
-
|
|
Gender
|
|
|
|
Female
|
68
|
73
|
|
Male
|
24
|
26
|
|
Other
|
1
|
1
|
|
Age
|
|
|
|
22-25
|
49
|
53
|
|
26-29
|
30
|
32
|
|
30-33
|
9
|
10
|
|
34-37
|
4
|
4
|
|
38+
|
1
|
1
|
|
Race/ethnicity of participants identifying as URM (n=34 responses)
|
|
Hispanic or Latinx only
|
16
|
47
|
|
Asian or Pacific Islander only
|
7
|
21
|
|
Black or African American only
|
4
|
12
|
|
White
|
3
|
9
|
|
Both Asian or Pacific Islander, and Hispanic or Latinx
|
2
|
6
|
|
Both Black or African American, and White
|
1
|
3
|
|
Indigenous only
|
1
|
3
|
|
Pre-COMET clinical experience* (n=219 responses)
|
|
Shadowing
|
67
|
72
|
|
Clinical volunteering
|
57
|
61
|
|
Research
|
47
|
51
|
|
Health care aids
|
13
|
14
|
|
Medical scribe
|
12
|
13
|
|
Technician (eg, emergency medical, lab, radiology)
|
8
|
9
|
|
Other/none
|
15
|
16
|
|
Reported educational trajectory at time of enrollment in COMET* (n=138 responses)
|
|
Medical school - MD program
|
61
|
66
|
|
Medical school - DO program
|
26
|
28
|
|
Physician assistant - PA program
|
25
|
27
|
|
Nurse practitioner school - NP program
|
8
|
9
|
|
Master of public health - MPH program
|
6
|
6
|
|
Doctor of philosophy - PhD program
|
4
|
4
|
|
Nursing school - RN program
|
2
|
2
|
|
Other programs
|
6
|
6
|
|
*Select all that apply question Abbreviations: COMET, Stanford Medical Scribe Fellowship; URM, underrepresented in medicine.
|
Sixty-nine percent (64/93) of all respondents and 68% (23/34) of URM respondents reported applying to a health professional school. Seventy percent (45/64) of all respondents and URM respondents (16/23) who applied reported being accepted. Among self-reported acceptance into a health professional school, 84% (38/45) were accepted within 1 year and 16% (7/45) were accepted within 2 to 3 years of completing COMET. For MD/DO and PA/NP programs, overall acceptance rates were 51% (24/47) and 61% (11/18), respectively; and URM acceptance rates were 43% (3/7) and 58% (7/12), respectively. COMET’s acceptance rates are higher than the national rates for MD/DO/PA/NP programs among all applicants (Figure 1).
Of the 29 respondents who had not applied to a health professional school at the time of survey completion, 59% (17/29) were “planning to apply to a health professional school,” 31% (9/29) were “currently applying to a health professional school this cycle,” 7% (2/29) were “not planning to apply at this time,” and 3% (1/29) were “accepted to a health professional school prior to COMET.”
Of the 11 URM respondents who had not applied to a health professional school at the time of survey completion, 55% (6/11) are “planning to apply to MD/DO school,” 18% (2/11) are “currently applying to MD/DO school this cycle,” 18% (2/11) are “planning to apply to PA/NP school,” and 9% (1/11) have “changed career paths and are pursuing an MBA.”
For respondents currently in or recently graduated from a health professional school, 71% (27/38) “strongly agreed” and 26% (10/38) “agreed” that COMET helped them succeed in their classes, clinical clerkships, research/scholarly projects, and/or overall training and skills at school. When asked an optional free response question on how they perceived COMET helped their educational trajectory, participants most frequently reported faculty mentorship and clinical experience as influential factors (63%, 41/65 responses).
We found no statistically significant associations, including acceptance rates among race/ethnic categories (P=.37) or URM status (P=.88), between participant demographics and responses with self-reported acceptance at a health professional school. Stratifying for MD/DO schools only, a χ2 test for URM versus non-URM acceptances was statistically nonsignificant (P=.64).
While significant research is available on the benefits of having a medical scribe for clinicians, sparse literature exists on the effects of medical scribing on the educational trajectory of prehealth students. To our knowledge, this is the first study to assess the impact of a postbaccalaureate medical scribing program on its prehealth participants’ educational goals, preparation for graduate training, and acceptance into health professional schools—with a particular focus on its URM alumni.
We found an association between COMET and a positive impact on educational trajectory and a higher acceptance rate into MD/DO and PA/NP programs than the national rates for both overall and URM applicants. While selection bias is a potential confounder (ie, motivated prehealth students who sought out COMET could have achieved their goals on their own), our assessment revealed—through participants’ perceptions about the impact of COMET on their educational trajectory and how soon after completing COMET they reported being accepted to a health professional school—that more likely than not, COMET played a positive role.
The benefits of medical scribing for URM learners are particularly notable because they face unique challenges in applying to health professional schools. URMs comprise only 8% through 13% of medical school matriculants 22, 23; among medical students, Hispanics are underrepresented by 70% relative to the age-adjusted US population, Black males by 60%, and Black females by 40%. 24, 25 Future research could investigate whether intentional recruitment and support of URM scribes leads to higher numbers of URM matriculants or whether scribe placement in critical shortage specialties (eg, family medicine) or underserved clinical settings (eg, rural) leads to higher numbers of students interested in those careers. Postbaccalaureate scribing programs may serve as pipeline development for prehealth students and may help increase the diversity of the future health care workforce.
Acknowledgments
The authors thank Anthony Duong, MPH, program manager at the time this report was written and all the scribes and faculty of the Stanford Medical Scribe Fellowship.
References
-
Gidwani R, Nguyen C, Kofoed A, et al. Impact of scribes on physician satisfaction, patient satisfaction, and charting efficiency: A randomized controlled trial. Ann Fam Med. 2017;15(5):427-433. doi: 10.1370/afm.2122
-
Gottlieb M, Palter J, Westrick J, Peksa GD. Effect of medical scribes on throughput, revenue, and patient and provider satisfaction: A systematic review and meta-analysis. Ann Emerg Med. 2021;77(2):180-189. doi:10.1016/j.annemergmed.2020.07.031
-
Ullman K, McKenzie L, Bart B, et al. The effect of medical scribes in emergency departments: A systematic review. JEM J Emerg Med. 2021;61(1):19-28. doi:10.1016/j.jemermed.2021.02.024
-
Ziemann M, Erikson C, Krips M. The use of medical scribes in primary care settings: A literature synthesis. Med Care. 2021;59(Suppl 5):S449-S456. doi:10.1097/MLR.0000000000001605
-
Abdulahad D, Ekpa N, Baker E, et al. Being a medical scribe: good preparation for becoming a doctor. Med.Sci.Educ. 2020;30(1):569-572. doi:10.1007/s40670-020-00937-w
-
Hewlett WH, Woleben CM, Alford J, Santen SA, Buckley P, Feldman M. Impact of scribe experience on undergraduate medical education. Med Sci Educ. 2020;30(4):1363-1366. doi:10.1007/s40670-020-01055-3
-
DeWitt D, Harrison LE. The potential impact of scribes on medical school applicants and medical students with the new clinical documentation guidelines. J Gen Intern Med. 2018;33(11):2002-2004. doi:10.1007/s11606-018-4582-8
-
Lin S, Duong A, Nguyen C, Teng V. Five years’ experience with a medical scribe fellowship: shaping future health professions students while addressing provider burnout. Acad Med. 2021;96(5):671-679. doi:10.1097/ACM.0000000000003757
-
Gellert GA, Ramirez R, Webster SL. The rise of the medical scribe industry: implications for the advancement of electronic health records. JAMA. 2015;313(13):1315. doi:10.1001/jama.2014.17128
-
Andriole DA, Jeffe DB. Characteristics of medical school matriculants who participated in postbaccalaureate premedical programs. Acad Med. 2011;86(2):201-210. doi:10.1097/ACM.0b013e3182045076
-
Romero R, Miotto K, Casillas A, Sanford J. Understanding the experiences of first-generation medical students: Implications for a diverse physician workforce. Acad Psychiatry. 2020;44(4):467-470. doi:10.1007/s40596-020-01235-8
-
Roche R, Manzi J, Baker S, Ndubuizu T. Under‐represented minority students and identification of obstacles to a career in medicine. Clin Teach. 2021;18(2):186-190. doi:10.1111/tct.13312
-
-
Association of American Medical Colleges. Table A-14.1: Race/Ethnicity Responses (Alone and In Combination) of Applicants to U.S. MD-Granting Medical Schools, 2017-2018 through 2021-2022. November 12, 2021. Accessed April 18, 2022.
https://www.aamc.org/media/6051/download?attachment
-
Association of American Medical Colleges. Table A-14.3: Race/Ethnicity Responses (Alone and In Combination) of Matriculants to U.S. MD-Granting Medical Schools, 2017-2018 through 2021-2022. November 12, 2021. Accessed April 18, 2022.
https://www.aamc.org/media/8826/download?attachment
-
-
-
-
-
-
Elo S, Kyngas H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107-115. doi: 10.1111/j.1365-2648.2007.04569
-
Acosta D, Poll-Hunter N, Eliason J. Trends in racial and ethnic minority applicants and matriculants to U.S. medical schools; 1980-2016. Association of American Medical Colleges. November 2017. Accessed October 26, 2022.
https://www.aamc.org/media/8816/download
-
-
Lett E, Murdock HM, Orji WU, Aysola J, Sebro R. Trends in racial/ethnic representation among US medical students. JAMA Netw Open. 2019;2(9):e1910490. doi: 10.1001/jamanetworkopen.2019.10490
-
Abdulrazzak A, Chandler A, Lu R, et al. Mini-medical school programs decrease perceived barriers of pursuing medical careers among underrepresented minority high school students. J Osteopath Med. 2021;121(12):883-890. doi: 10.1515/jom-2021-0125



There are no comments for this article.