Introduction: As the COVID-19 pandemic affected the ability to conduct in-person sessions to teach clinical skills, our medical school developed a curriculum to introduce first-year medical students to telemedicine visits, while also reinforcing their history-taking and clinical reasoning skills.
Methods: All first-year medical students at Florida Atlantic University went through three sessions on telemedicine that began with a lecture, followed by a standardized patient interaction, then a small group meeting with clinical faculty. We assessed the sessions using survey questions on a 5-point Likert scale and additional narrative feedback. We also assessed students on a telemedicine objective structured clinical examination (OSCE) at the end of the semester and compared results to the previous year’s same case done in person.
Results: Students overall found the sessions helpful for refining their history-taking skills and that the knowledge gained would be helpful in their future practices. They felt the online platform was a useful way to interact with patients, but had frustrations with technical difficulties. They also expressed a greater appreciation for the ability to perform an in-person physical examination. Students performed similarly on the OSCE station in person compared to virtual visits (mean score 93% vs 93.75%).
Conclusion: Introducing telemedicine during a first-year medical school clinical skills course provides students with opportunities to refine their clinical skills while introducing a skill that will be commonplace in the postpandemic environment. This curriculum could be adopted not only during a time of necessary distance learning, but also continued as in-person education resumes.
In the 2017-2018 academic year, 85 of 147 medical schools in the United States offered telemedicine, either through required or elective courses, with most of these being in the clerkship phase.1 In the preclerkship phase, 59% of schools utilize standardized patients to teach telemedicine, while 71% use didactic approaches2,3 However, there is a paucity of data describing the effectiveness of these approaches. Telemedicine has had a steady increase in use since 2005 where there were approximately 0.020 per 1,000 patients using the services compared to 6.57 per 1,000 in 2017.4 This represents a steady increase of about 52% per year. With the COVID-19 pandemic, one large academic institution saw an increase of 683% of daily telemedicine use for urgent care.5 With this significant surge in telemedicine and the transition to distance learning, an opportunity to incorporate telemedicine into medical school curricula not only makes sense, but has also become a necessity.
Currently, there are no competencies or standardized ways to assess a telemedicine visit in the preclerkship phase of medical school. In order to assess students conducting telemedicine visits and to teach them how to avoid common pitfalls, we created a Virtual Communication Checklist that can be used as benchmarks for telemedicine visits. Guided by these benchmarks, we created sessions that reinforced students’ history-taking skills and introduced them to new skills necessary for effective telemedicine visits.
Prior to COVID-19, first-year medical students at Florida Atlantic University participated in the Foundations of Medicine Clinical Skills course on a weekly basis. Students would interview a standardized patient (SP) face to face with feedback from a faculty member, then submit a history and physical note to a faculty member for feedback. The following week, students presented the case in a small group led by clinical faculty. These “clinical learning groups” provided students with the opportunity to discuss clinical reasoning, communication skills, and systems-based practice.
In order to adjust the curriculum due to the restrictions associated with the COVID-19 pandemic and the necessity for remote learning, the SP sessions that had been previously used were converted to telemedicine cases, with addition of a specific didactic session on how to conduct a telemedicine encounter. Each of these SP sessions were followed by virtual small-group sessions 1 week later for reflection. The first SP session began with a 30-minute, lecture-based introduction to the techniques of interviewing a patient via telemedicine (Figure 1) and demonstrated the benefits and limitations of virtual visits. The students then proceeded to an SP scenario that was built around abdominal pain, that also followed the students’ concurrent pathophysiology course. Students would interview an SP through an online platform in groups of two students with faculty observing and providing feedback at the end of the interview. Following each SP session, students documented and submitted a note to a faculty member for review. The students and faculty then met 1 week later in groups of eight to discuss, further develop reasoning skills, and reflect on telemedicine encounters. The next SP encounter covered interviewing a pediatric patient, and the third SP encounter implemented motivational interviewing in a patient who had gained weight and increased their alcohol consumption.
Evaluations from the students were collected in order to assess the ability of the virtual medicine encounter sessions to teach appropriate telemedicine clinical skills. Students were also evaluated via an end-of-semester objective structured clinical examination (OSCE) to assess that they successfully performed the benchmarks expected of them.
The Institutional Review Board at Florida Atlantic University reviewed and approved this research.
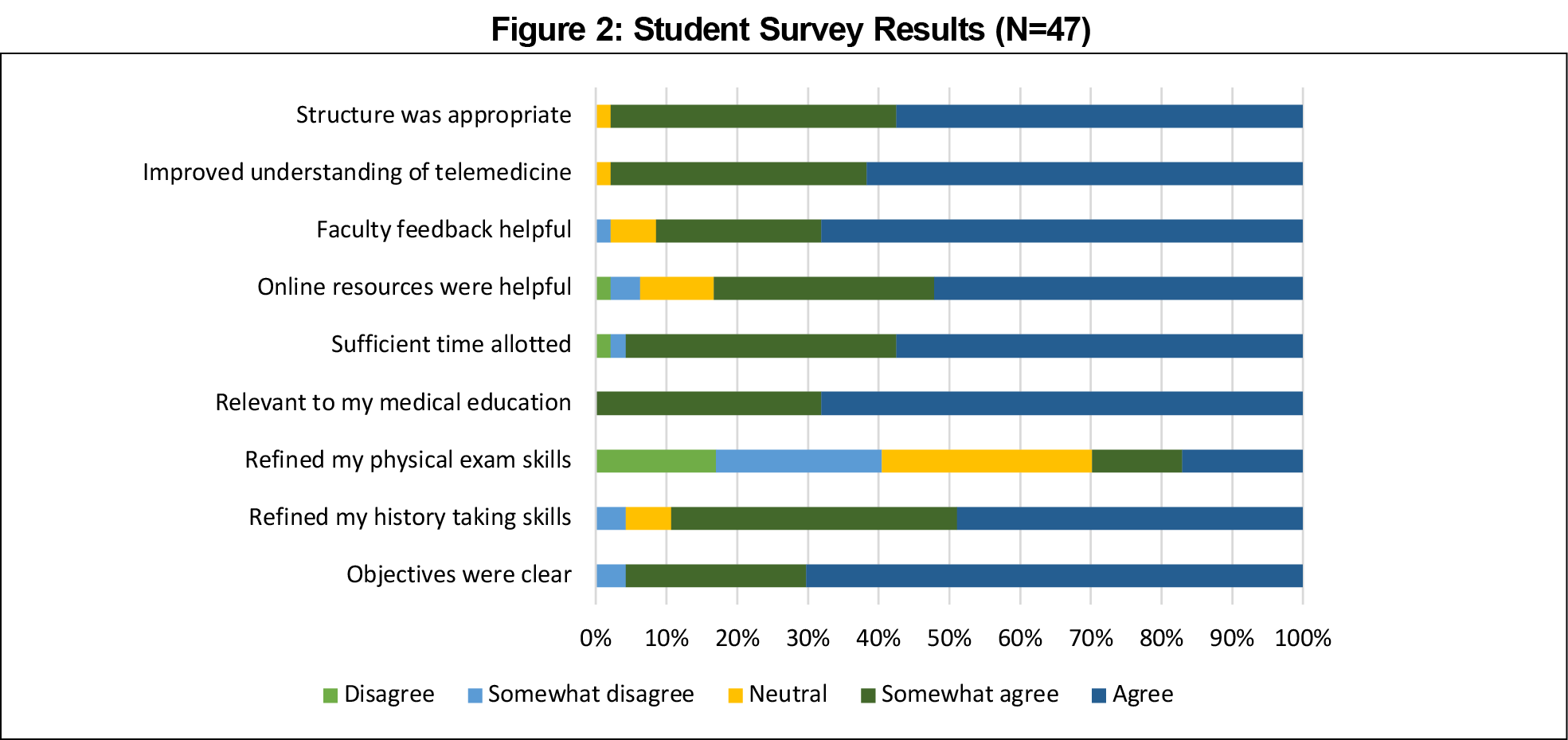
Using a 5-point Likert scale, we collected evaluations from students who participated in the sessions (N=47). Students evaluated the ability of the telemedicine sessions to refine their history-taking skills and ranked it with an average of 4.33. Students felt the topic of telemedicine was relevant to their medical education with an average score of 4.68. Students ranked the ability of the sessions to help refine their physical exam skills as an average of 2.89. Figure 2 shows the results of all survey questions.
After coding narrative feedback and identifying themes, the most common theme represented within the surveys conveyed that the students felt the telemedicine curriculum enforced the importance of the physical exam and made evident the difficulties that performing a patient encounter over a video platform would bring. However, a large subset of students felt that these sessions helped them improve upon their ability to acquire pertinent medical information over a video platform. Participants also stressed the convenience of meeting a patient over a video platform but expressed frustration with technical difficulties. Lastly, the students felt the benchmarks (Figure 1) were an important element in conducting a productive telemedicine encounter and would be an important skill in the practice of medicine during the pandemic and after. Students highly valued the postsession as a place to discuss clinical reasoning and apply medical knowledge to a case.
Following completion of these formative sessions, we assessed students on their performance of the benchmarks in a telemedicine OSCE. The virtual OSCE was structured similarly to previous years, with some modifications due to the virtual nature, including the addition of expectations for a telemedicine encounter, as well as modification of physical exam expectations. Students averaged a score of 93% on these stations. Previous-year OSCEs that were conducted in person averaged 93.5%, making the effectiveness of using these resources to teach students through a virtual, remote platform on par with the in-person sessions.
With telemedicine visits having come to the forefront of medicine due to the COVID-19 pandemic, physicians will likely continue to increase access by including more telemedicine visits as part of their practice. Therefore, it is crucial to educate students on the appropriate way to conduct virtual visits during their preclerkship curriculum. Our curriculum had clear objectives and informative content including benchmarks. The use of faculty during SP sessions and after was seen as helpful. The virtual visits and sessions were found to be well structured to allow students to practice and hone their telemedicine skills.
Limitations to this curriculum included a lack of further development of physical exam skills. This is a common issue with telemedicine visits and can be improved by helping students better understand how to tailor their exam skills to a telemedicine visit. The development of the Virtual Medicine Encounter Benchmarks was crucial in guiding students on the appropriate components of a telemedicine visit in their first-year clinical skills course. This could easily be implemented at other schools who currently use standardized patient sessions and wish to introduce telemedicine in the preclerkship phase.
References
- Liaison Committee on Medical Education. LCME annual medical school questionnaire Part II, 2013-2014 through 2018-2019.
- Pathipati AS, Azad TD, Jethwani K. Telemedical Education: Training digital natives in telemedicine. J Med Internet Res. 2016;18(7):e193. doi:10.2196/jmir.5534
- Waseh S, Dicker AP. Telemedicine training in undergraduate medical education: mixed-methods review. JMIR Med Educ. 2019;5(1):e12515. doi:10.2196/12515
- Barnett ML, Ray KN, Souza J, Mehrotra A. Trends in telemedicine use in a large commercially insured population, 2005-2017. JAMA. 2018;320(20):2147-2149. doi:10.1001/jama.2018.12354
- Mann DM, Chen J, Chunara R, Testa PA, Nov O. COVID-19 transforms health care through telemedicine: evidence from the field. J Am Med Inform Assoc. 2020;27(7):1132-1135. doi:10.1093/jamia/ocaa072




There are no comments for this article.