Introduction: Opioid use disorder (OUD) remains a critical public health concern, and primary care physicians are essential to its identification and treatment. However, many residency programs lack structured training in evidence-based behavioral and pharmacologic approaches to OUD. This study evaluated the impact of an asynchronous, video-based OUD curriculum on knowledge acquisition among first-year family medicine residents.
Methods: We used a quasi-experimental design to assess the feasibility and short-term impact of an OUD curriculum adapted from MedEdPORTAL. Twenty first-year residents completed the curriculum during a 2-week behavioral health rotation and were assessed using a 10-question pretest and a 20-question posttest. A control group of nine third-year residents completed only the posttest. All assessments were administered electronically. Due to anonymous response collection, pre- and posttest scores could not be matched. We used Mann-Whitney U tests to compare posttest scores between groups and pre- versus posttest scores within the intervention group. We also calculated effect sizes.
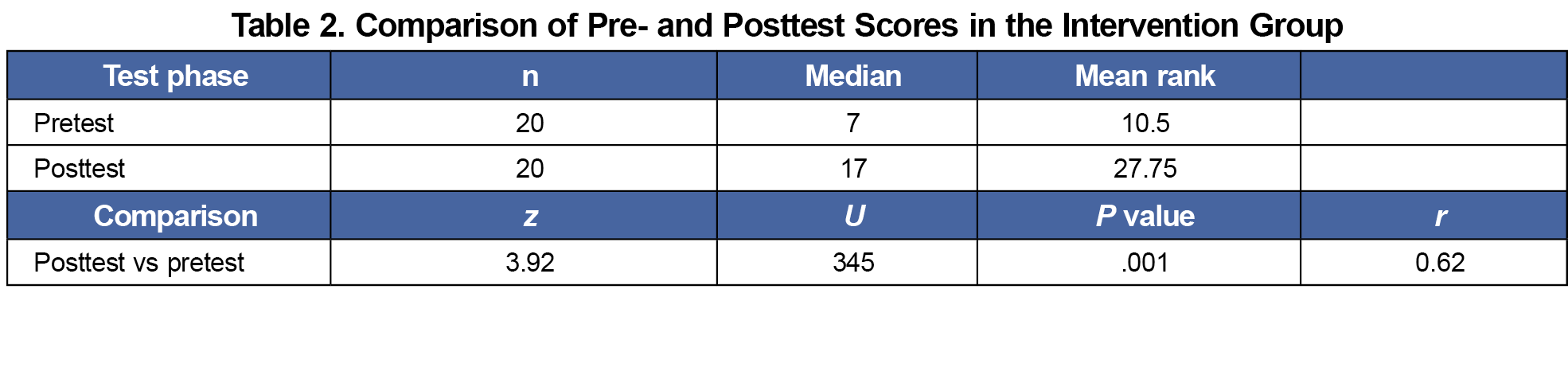
Results: Residents who completed the curriculum demonstrated a significant increase in knowledge from pretest (median=7.0) to posttest (median=17.0), U=345.0, P<.001. A large effect size (r=0.62) indicated a substantial gain in knowledge following the curriculum
Conclusions: An asynchronous OUD curriculum significantly improved resident knowledge and demonstrated comparable posttest performance to a control group of senior residents, suggesting noninferiority to traditional training approaches and supporting the curriculum’s potential as a scalable educational model.
Opioid use disorder (OUD) continues to pose challenges to US health care systems, with more than 9 million Americans affected and an estimated 4.4% of prescribed opioids misused.1,2 Legislative efforts have sought to limit opioid prescribing, yet many primary care providers report inadequate training in screening, assessment, and treatment of OUD.3-5 Evidence-based tools such as the Drug Abuse Screening Test (DAST-10), Screening, Brief Intervention, and Referral to Treatment (SBIRT), and Motivational Interviewing (MI) support provider-patient communication about opioid use and are effective frameworks for guiding treatment planning.6,7 However, these tools are underutilized in primary care, in part due to limited educational exposure during residency training.8,9
To address this gap, we implemented an open access, asynchronous video-based OUD curriculum originally developed by Spangler et al with first-year family medicine residents at an academic medical center. The curriculum incorporates video vignettes that demonstrate MI and SBIRT techniques and emphasize both psychopharmacologic and behavioral approaches to OUD care.10
This study aimed to evaluate whether this online curriculum improved residents’ knowledge related to OUD assessment and management in primary care settings.
Curriculum
This project used a quasi-experimental design to evaluate the impact of an asynchronous OUD curriculum on the knowledge of first-year family medicine residents at an academic medical center. The curriculum, adapted from Spangler et al, included approximately 5 hours of online, self-paced modules and video case vignettes. These vignettes demonstrated the application of key evidence-based tools for engaging patients in OUD-related discussions, including the DAST-10, SBIRT framework, and MI.10
Procedure
The curriculum was implemented throughout residents’ first year during a 2-week behavioral health rotation. Residents in the intervention group (n=20) completed a 10-item multiple-choice pretest prior to beginning the modules and a 20-item multiple-choice posttest following completion. The control group (n=9), graduating third-year residents who did not receive the curriculum, completed the 20-item posttest during the final months of their third year. Assessments were administered electronically using REDCap (Solera Holdings). The assessment items measured applied knowledge across content domains, including (a) identification of OUD symptoms, (b) use of validated screening tools and Centers for Disease Control and Prevention (CDC) guidelines, (c) core principles of motivational interviewing, and (d) appropriate use of medication-assisted treatment, including buprenorphine/naloxone. Example questions included
- The 2022 CDC Clinical Practice Guidelines for Prescribing Opioids for Pain recommend patients receiving chronic opioid therapy be seen at least how often for opioid assessment? and
- The decisional balance tool in Motivational Interviewing helps explore what?
The full set of assessment items is available in Appendices A and B, as well as in the Society of Teachers of Family Medicine Resource Library.16
Data Analysis
Due to anonymity protocols, individual pre- and posttest scores could not be matched. All analyses were conducted at the group level. Because the data were not normally distributed, we used Mann-Whitney U tests to compare (a) posttest scores between the intervention and control groups, and (b) pre- and posttest scores within the intervention group. We calculated effect sizes (r) using the formula r=z/√N, where z is the standard score and N is the total sample size. We reported median values as measures of central tendency. We used a two-tailed α level of .05 for all statistical tests. The project was assessed by the authors’ institutional review board and deemed exempt from review under IRB00051066. Although this study was not designed as a formal noninferiority trial, the between-group comparison was interpreted through a noninferiority lens, consistent with reviewer feedback and the educational context of the intervention.
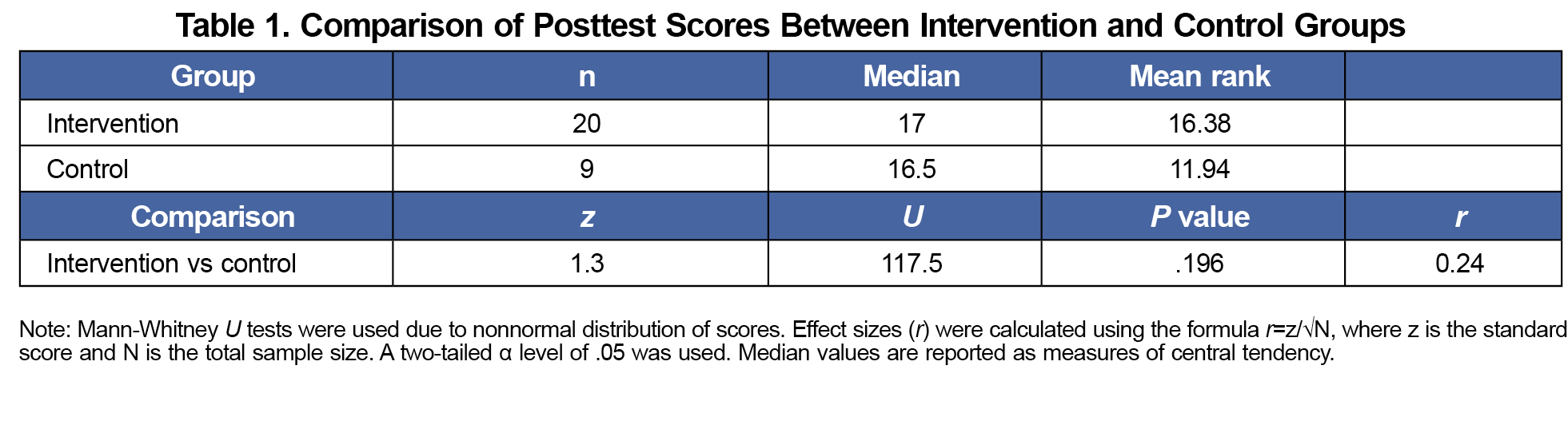
Twenty first-year residents completed the OUD curriculum and both assessments, while nine residents served as controls. Posttest scores in the intervention group (median=17.0) were comparable to those of the control group (median=16.5) with a small difference. However, the difference was not statistically significant (U=117.5, P=.196), with a small effect size (r=0.24) that supports a noninferiority interpretation, indicating that the asynchronous curriculum may be at least as effective as traditional training received by senior residents (Table 1).
Within the intervention group, scores significantly increased from pretest (median=7.0) to posttest (median=17.0), U=345.0, P<.001. This increase reflects a large effect size (r=0.62), indicating a substantial gain in knowledge following the curriculum (Table 2).
The lack of a statistically significant difference in posttest scores between the intervention and control groups, combined with a small-to-moderate effect size, supports a noninferiority interpretation. Additionally, the implementation of an asynchronous, video-based OUD curriculum for first-year family medicine residents was associated with a significant increase in knowledge related to screening, assessment, and treatment of OUD. The large pretest to posttest effect size suggests that the curriculum was effective in conveying both behavioral and pharmacologic concepts central to primary care-based OUD management. Together, these findings suggest that the asynchronous curriculum may be at least as effective as traditional instruction, offering a flexible and scalable alternative for residency programs seeking to meet Accreditation Council for Graduate Medical Education training requirements in OUD care.
These findings are consistent with existing literature emphasizing the need for OUD-specific training that includes practical tools such as DAST-10, SBIRT, and MI.11,12 The asynchronous nature of this curriculum provided scheduling flexibility while maintaining exposure to relationally focused skills that are critical for engaging patients with substance use concerns.13 Given growing efforts to expand access to medication-assisted treatment in primary care, integration of this type of training into residency education may support future workforce preparedness and contribute to reducing treatment gaps.14,15
This study was designed as a feasibility evaluation of a scalable, asynchronous curriculum. While our findings demonstrate short-term knowledge gains, we did not assess behavioral outcomes such as clinical documentation, referrals, or prescribing practices. Assessing these outcomes is an important next step for future research. Further, this study is limited by its small sample size and inability to link individual pre- and posttest scores, which prevented use of paired analyses. In addition, the assessment tool was developed locally and has not been formally validated. Results should be interpreted as preliminary and exploratory. Future research should assess long-term retention of knowledge, impact on clinical behavior, and applicability across institutions and learner levels.
This study demonstrates that an asynchronous, evidence-based curriculum can significantly improve resident knowledge related to OUD in a short period of time. Incorporating flexible, case-based training in SBIRT, MI, and medication-assisted treatment into residency education may better prepare future family physicians to address substance use in primary care. Continued curriculum refinement and evaluation will be essential to supporting competency-based education in OUD treatment across diverse training environments. Integrating such scalable, evidence-based content into routine residency training may help meet the ongoing workforce needs in OUD treatment.
Acknowledgments
Presentation:
This study was previously presented as follows:
Johnson, DJ, Kirk, JK. Building an Opioid Use Disorder Curriculum for Family Medicine Residents. Roundtable at the Society of Teachers of Family Medicine Annual Conference, May 3, 2025, Salt Lake City, UT.
References
- Dowell D, Brown S, Gyawali S, et al. Treatment for opioid use disorder: population estimates—United States, 2022. Morb Mortal Wkly Rep. 2024;73(25):567-574. doi:10.15585/mmwr.mm7325a1
- Mojtabai R, Amin-Esmaeili M, Nejat E, Olfson M. Misuse of prescribed opioids in the United States. Pharmacoepidemiol Drug Saf. 2019;28(3):345-353. doi:10.1002/pds.4743
- Randall DJ, Vanood A, Jee Y, Moore DD. National and state level opioid-restricting legislation in total joint arthroplasty: a systematic review. J Arthroplasty. 2022;37(1):176-185. doi:10.1016/j.arth.2021.07.013
- Davis CS, Lieberman AJ. Laws limiting prescribing and dispensing of opioids in the United States, 1989-2019. Addiction. 2021;116(7):1,817-1,827. doi:10.1111/add.15359
- Kirane H, Drits E, Ahn S, et al. Addressing the opioid crisis: an assessment of clinicians’ training experience, practices, and attitudes within a large healthcare organization. J Opioid Manag. 2019;15(3):193-204. doi:10.5055/jom.2019.0503
- Agerwala SM, McCance-Katz EF. Integrating screening, brief intervention, and referral to treatment (SBIRT) into clinical practice settings: a brief review. J Psychoactive Drugs. 2012;44(4):307-317. doi:10.1080/02791072.2012.720169
- Petrides J. Motivational interviewing in primary-care: substance use disorders beyond AUDIT/DAST. Prim Care. 2023;50(1):1-10. doi:10.1016/j.pop.2022.10.009
- Agley J, Gassman RA, DeSalle M, Vannerson J, Carlson J, Crabb D. Screening, brief intervention, referral to treatment (SBIRT), and motivational interviewing for PGY-1 medical residents. J Grad Med Educ. 2014;6(4):765-769. doi:10.4300/JGME-D-14-00288.1
- Wamsley MA, Julian KA, O’Sullivan P, et al. Designing standardized patient assessments to measure SBIRT skills for residents. J Alcohol Drug Educ. 2013;57(1):46-65.
- Spangler JG, Shull CN, Hildebrandt CA, et al. Opioid use disorder and assessment of patient interactions among family medicine residents, medical students, and physician assistant students. MedEdPORTAL. 2020;16:11012. doi:10.15766/mep_2374-8265.11012
- Sokolski E, Buchheit BM, Desai S, Englander H. It’s time to train residents in addiction medicine. J Grad Med Educ. 2023;15(6):632-637. doi:10.4300/JGME-D-23-00317.1
- Evans T, Morphew J, Gu J, Hiefner A, McGregor T, Jochim A. Bup-ing up residency: a dose of change for OUD care. Annals Fam Med. 2024; 22(Suppl1):7164. doi:10.1370/afm.22.s1.7164
- Zoorob R, In Kim-Vences S, Hirth JM, et al. Asynchronous online training increased knowledge, confidence, and intent to screen and treat substance use disorders among primary care clinicians practicing in Texas. Prev Med. 2024;185:108038. doi:10.1016/j.ypmed.2024.108038
- Cheng H, McGovern MP, Garneau HC, et al. Expanding access to medications for opioid use disorder in primary care clinics: an evaluation of common implementation strategies and outcomes. Implement Sci Commun. 2022;3(1):72. doi:10.1186/s43058-022-00306-1
- Gardner-Buckshaw SL, Perzynski AT, Spieth R, et al. Increasing primary care utilization of medication-assisted treatment (MAT) for opioid use disorder. J Am Board Fam Med. 2023;36(2):251-266. doi:10.3122/jabfm.2022.220281R2
- STFM Resource Library. Society of Teachers of Family Medicine. Accessed September 10, 2025. https://resourcelibrary.stfm.org/home



There are no comments for this article.