Background and Objectives: Primary care physicians (PCPs) are front line providers of musculoskeletal (MSK) care and MSK injections. Little is known about the volume of common MSK injections performed by FM residents (FMRs) and those residents participating in a longitudinal clinical sports medicine (SM) track. This study outlines an SM track and demonstrates the MSK procedural experience of SM track residents (SMRs) and traditional FMRs (non-SMRs).
Methods: We utilized a retrospective study design. We compared billing codes and provider information for common MSK injections for the second (PGY-2) and third (PGY-3) postgraduate years for non-SMRs (n=39) and SMRs (n=7) graduating between 2018-2021. We used the average number of patient encounters for each comparison group (non-SMRs vs SMRs) to determine the percentage of patients receiving an MSK injection in each cohort by PGY status.
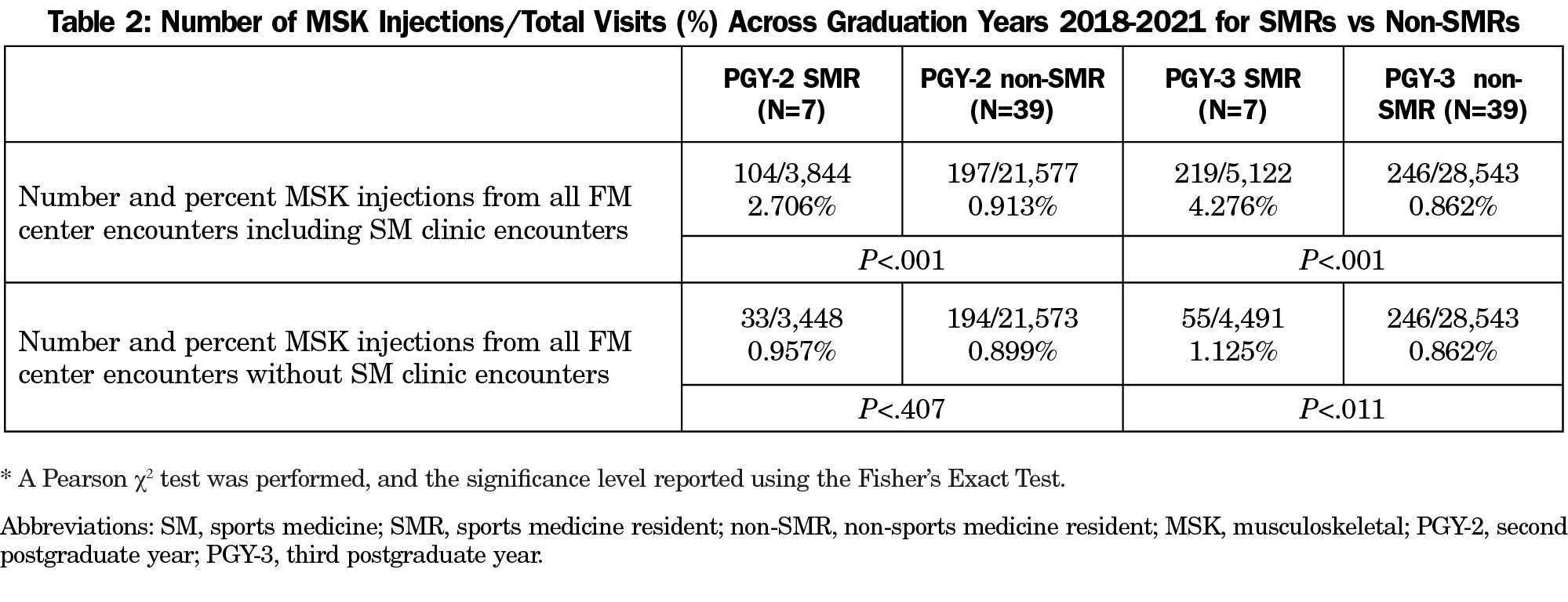
Results: Of patients receiving MSK injections across both groups, the most common was the landmark-guided large joint injection (64.23%), and the most frequent site was the knee (47.00%). SMRs performed significantly more MSK injections per patient evaluated compared to non-SMRs while in the SM clinic (PGY-2: 2.706% vs 0.913%, P<.001; PGY-3: 4.276% vs 0.862%, P<.001). No significant differences existed between PGY-2 groups when the influence of the SM clinic was removed, but PGY-3 SMRs performed significantly more injections than PGY-3 non-SMRs (1.225% vs 0.862%, P<.011).
Conclusions: An SM track in the FM residency is associated with an increased volume of MSK injections among SMRs compared to their graduate year-matched non-SMRs.
Guidelines exist for MSK and sports medicine (SM) education in family medicine (FM) residencies including training in common musculoskeletal (MSK) injections.1-3 Per national FM residency survey data, 89% of graduating FM residents (FMRs) felt prepared to perform joint aspiration and injection, and 17% felt prepared to use MSK ultrasound.4 To our knowledge, there is no prior literature on the development of a longitudinal SM clinical track for FMRs that leverages an academic SM clinic as a training site. Further, the number of common MSK injections performed by FMRs in routine continuity encounters versus a longitudinal SM track remains unknown.
Our study addresses this gap in the literature, describes the feasibility of a longitudinal SM track for FMRs in the second and third postgraduate year (PGY2, PGY3), and evaluates the impact of this education on the volume of MSK injections performed by residents participating in the SM track (SMRs) versus non-SM track FMRs (non-SMRs).
Program Setting and Features
An SM track was established to augment FMR MSK training within an SM clinic in a university-based FM center with 12 residents per year. SMRs are selected through an internal application process during their first postgraduate year (PGY-1). Following this, 1 half day of FM clinic per week is replaced with SM clinic, precepted by fellowship-trained SM physicians. The SM clinic receives patients through self-referral from the FM center and referral from internal and external (orthopedics, physical medicine and rehabilitation, neurology, and outside primary care) sources. Patients referred from non-primary care specialties are not scheduled in SMR clinics due to anticipated patient complexity. SMRs are expected to perform injections on their patient panel with physician oversight.
Research Design and Methods
The study utilized a retrospective cohort design after receiving institutional review board exemption, with the SM track as the exposure and the percentage of encounters with an MSK injection as the outcome. Participating residents graduated between 2018-2021, and SMRs were compared with non-SMRs using billing, coding, and provider data. Resident demographics, number of patient encounters, and number of clinic sessions were reported.
SM faculty identified the most common MSK injections by Current Procedural Terminology (CPT) codes as follows: injections of large (CPT CPT 20611; CPT 20610), medium (CPT 20606; CPT 20605), and small joints (CPT 20604; CPT 20600) with and without ultrasound (US) guidance; injection of the carpal tunnel (CPT 20526); trigger point injections (CPT 20552; CPT 20553); and trigger finger/tendon sheath injections (CPT 20550). Additional codes for the following injections were evaluated with few results and are combined in an “other injection” category: tendon origin/insertion injections (CPT 20551), injection of other peripheral nerve (CPT 64450), and tenotomy (CPT 24357).
We compared the percentage of encounters with completed MSK injections between the SMR and non-SMR cohorts and stratified based on residency year. Non-SMR cohorts represented traditional FMRs and served as control groups. We collected information regarding injected body parts.
Statistical Analysis
We analyzed data using SPSS (Version 27; IBM, Chicago, IL). We used a Pearson χ2 test and Fisher’s Exact test to compare the percentage of MSK injections in the two cohorts (SMRs vs non-SMRs).
Forty-six FMRs were included in the study, of which seven (15.2%) were enrolled in the SM track. FMRs were 59.0% female and 84.6% MD (15.4% DO), while SMRs were 42.9% female, and 28.6% MD (71.4% DO). The average number of SM clinic sessions staffed by SMRs was 30.6 (±6.6), with approximately six patients per clinic (5.81±2.85).
Of the patient encounters in which an MSK injection occurred (n=766), the most common site was the knee (47.00%) followed by the shoulder (25.20%). The most common injection was the landmark-guided large joint injection (64.23%). The average number of patient encounters per resident within the SMR and non-SMR groups in which an MSK injection was administered is shown in Figure 1. On average, 6% of patients evaluated in the SM clinic by a PGY-2 SMR received an MSK injection, which increased by PGY-3 (14.2%).
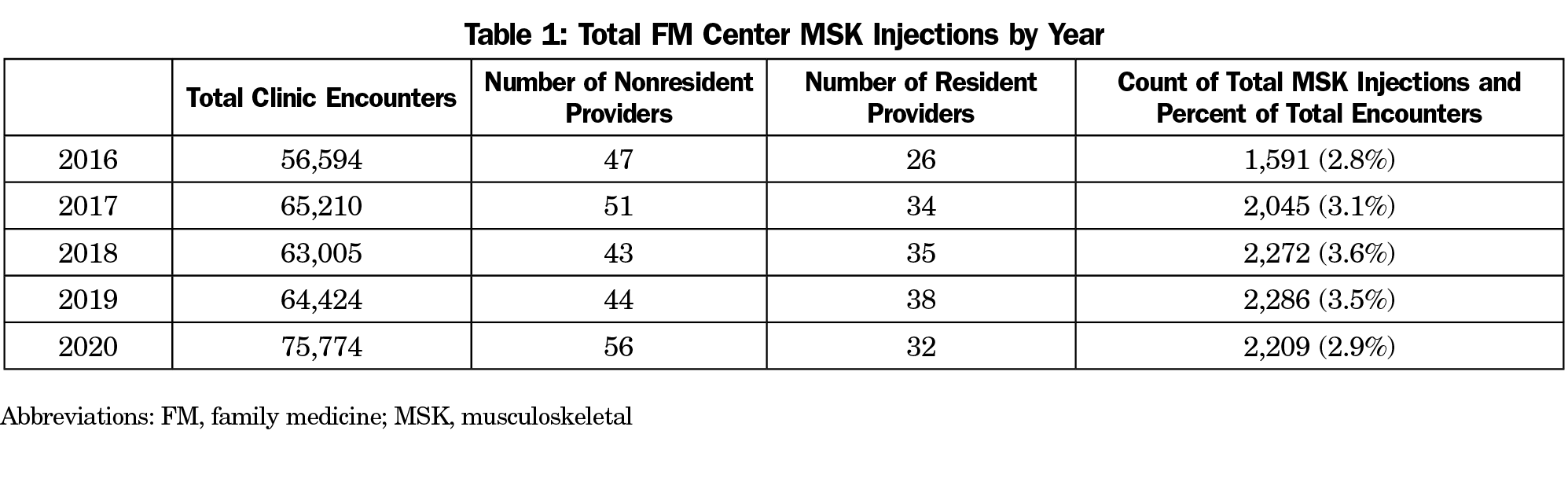
Table 1 shows total FM center encounters, including SM clinic encounters, and total number of visits where an MSK injection occurred; this demonstrates consistency in frequency of MSK injections. The percentage of patient encounters in which MSK injections were performed by trainee type and year are shown in Table 2. PGY-2 SMRs performed MSK injections on 2.706% of their evaluated patients, compared to 0.913% for non-SMRs (P<.001). This difference increased during PGY3 with 4.276% of SMR patients undergoing injections, versus 0.862% for PGY-3 non-SMRs (P<.001). When the influence of the SM clinic was removed from the data by examining only FM-based encounters, PGY-2 group differences were not significant, but by PGY3, SMRs were performing more injections than their peers regardless of clinic location (1.225% vs 0.862%, P<.011).
Our data indicate that SMRs participating in a longitudinal SM track perform more MSK injections compared with peers, suggesting that such a track is feasible for advancing procedural exposure. Additionally, most MSK injections performed by SMRs occur outside of the SM clinic. We also report average percentages of MSK injections for FMRs, which may serve as a benchmark for other FM residency programs.
Notable differences existed between the volume of injections performed in PGY2 and PGY3 for all FMRs, possibly due to increased clinic time in the PGY-3 year and improved confidence. Others have noted increased MSK knowledge in primary care residents who complete orthopedic rotations or have additional FM-based training.5-9 Our findings suggest that an additional SM longitudinal experience enhances opportunity for performing MSK injections.
Limitations to this study include the small sample size of SMRs, limited study period, and concern for generalizability of results to other programs or sites with different characteristics. The FM Department is unique in that it houses a separate SM clinic that may influence referral behaviors from internal FM providers. SMRs already held interest in SM, and this may have influenced MSK injection numbers. The use of billing and provider data to determine injection numbers may not capture all resident-performed injections. Differences in patient populations may lead to varying opportunities for MSK injections, and selection bias is inherent to the structure of the SM track; yet MSK injections remained higher for PGY-3 SMRs even when SM clinic encounters were removed to reflect only FM continuity encounters. Importantly, MSK injection volume and competency are independent metrics and should be measured separately.
An SM track for FMRs within an SM clinic can be successfully offered alongside traditional continuity clinic training, and increases the volume of MSK injections. Future directions for study should focus on confidence or objective knowledge assessments as well as observed evaluations of select MSK injections at the beginning and end of SM track training.
References
- Brennan FH Jr, Rao AL, Myers RA, et al. Suggested curricular guidelines for musculoskeletal and sports medicine in family medicine residency training. Curr Sports Med Rep. 2020;19(5):180-188. doi:10.1249/JSR.0000000000000713
- Recommended Curriculum Guidelines for Family Medicine Residents - Musculoskeletal and Sports Medicine. American Academy of Family Physicians. 2017. Accessed May 2, 2021. www.aafp.org/dam/AAFP/documents/medical_education_residency/program_directors/Reprint265_Musculo.pdf
- Sadikot C, Leung S, Vassilakis A, LeFrancois D. Addressing resident retention of musculoskeletal skills, knowledge, and confidence: a randomized controlled study of a clinic intervention. [published online ahead of print, 2021 Jan 26]. J Gen Intern Med. 2021;36(11):3595-3597. doi:10.1007/s11606-021-06595-x
- American Board of Family Medicine and Association of Family Medicine Residency Directors National Graduate Survey for Year. 2020. Accessed October 12, 2021. https://www.theabfm.org/sites/default/files/PDF/NationalOnly_Report2020.pdf
- Matheny JM, Brinker MR, Elliott MN, Blake R, Rowane MP. Confidence of graduating family practice residents in their management of musculoskeletal conditions. Am J Orthop. 2000;29(12):945-952.
- Haywood BL, Porter SL, Grana WA. Assessment of musculoskeletal knowledge in primary care residents. Am J Orthop. 2006;35(6):273-275.
- Deffenbacher B, Langner S, Khodaee M. Are self-study procedural teaching methods effective? a pilot study of a family medicine residency program. Fam Med. 2017;49(10):789-795.
- Seifert MK, Holt CT, Haskins A, Dexter W. Improving internal medicine resident comfort with shoulder and knee joint injections using an injection workshop. MedEdPORTAL. 2020;16:10979. Published 2020 Sep 28. doi:10.15766/mep_2374-8265.10979
- Pearson M, Barker AM, Battistone MJ, Bent S, Odden K, O’Brien B. Implementing an established musculoskeletal educational curriculum in a new context: a study of effectiveness and feasibility. Med Educ Online. 2020;25(1):1760466. doi:10.1080/10872981.2020.1760466




There are no comments for this article.