Background and Objectives: Vasectomy is considered a permanent contraceptive method with fewer associated harms than bilateral tubal ligation. However, the number of vasectomy-trained providers may not be meeting the demand for vasectomy in the United States. We describe the vasectomy training landscape in family medicine residencies and factors related to increased procedural training.
Methods: Program-specific data were collected from the Council of Academic Family Medicine Educational Research Alliance (CERA) national survey of family medicine program directors in 2019. Program characteristics, vasectomy training (eg, time spent, procedural numbers), as well as direct and specific faculty support are described, with bivariate analyses for factors related to procedural competency, defined as more than five vasectomy procedures per resident.
Results: We received responses from 250 program directors (response rate=39.8%), with representation across all US regions, and program types. Nearly half (47.5%) offered less than 1 day of vasectomy didactics and/or procedural training; 38.9% of programs reported having a family medicine faculty champion for vasectomy. Only 16 programs (6.8%) reported that their average graduating residents performed more than five vasectomies. Programs with a faculty champion (OR 28.1, CI 3.6-216.4) or family medicine faculty as primary trainer (OR 17.6, CI 2.2-138.2) were more likely to graduate residents who had performed more than five vasectomies.
Conclusions: Fewer than 10% of surveyed family medicine residency programs offer adequate vasectomy procedural training. Family medicine faculty who serve as primary trainers and act as faculty champions can increase vasectomy training opportunities for residents, and thereby increase the supply of vasectomy providers in the United States.
Family physicians, urologists, and obstetricians/gynecologists agree that vasectomy is more effective, safer, and less costly than bilateral tubal ligation.1 Despite these benefits, vasectomy is used by 7% of contraceptive users in the United States compared to female sterilization, which accounts for 22%.2 According to a survey of key US health care administrators and providers conducted in 2001 by the global women’s health nonprofit organization, EngenderHealth, one of the most frequent barriers to vasectomy services was a lack of trained providers.3
A US survey in 2002 reported that urologists perform the majority of vasectomies (79%) followed by family physicians (13%), and general surgeons (8%).4 Considering that family physicians comprise the second largest number of vasectomy-providing surgeons and are positioned to discuss pregnancy planning and prevention with patients and couples, vasectomy procedural training should be consistently included in their residency training. However, a 1989 survey of family medicine residency program directors on vasectomy training found that only 44% of programs had vasectomy training, 54% of them with both lecture and surgery, and the remaining with solely surgical training.5 Additionally, of programs with training available, only 22% of graduated residents reported performing more than 10 vasectomies during their residency.5 A 2003 national survey of family medicine chief residents showed that vasectomy was one of the least likely office procedures learned by residents, with only 17% reporting feeling somewhat competent at performing vasectomies and 54% reporting never having performed a vasectomy.6 In a 2011 national survey of family medicine program directors (n=220), 75.3% of program directors reported that their program offered vasectomy didactic training and 72.1% provided hands-on procedural training,7 though the training volume was not assessed.
The primary objective of this study was to characterize the current state of vasectomy procedural training across family medicine residency programs. As the establishment and maintenance of vasectomy training opportunities need to be prioritized, we surveyed family medicine program directors about the vasectomy training that their residents receive. The minimum volume of vasectomy experience for procedural competence was set at five procedures in the Council of Academic Family Medicine (CAFM) Consensus Statement for Procedural Training in Family Medicine Residency.8 Hence, our secondary objective was to examine the program-related factors associated with a resident having performed more than five vasectomies on average during residency.
We surveyed family medicine program directors about vasectomy training opportunities via the CAFM Educational Research Alliance (CERA) National Questionnaire, which is distributed biannually to allopathic and osteopathic family medicine residency program directors. The detailed methodology of the CERA Program Director Questionnaire is described in previous publications.9 The project was approved by the American Academy of Family Physicians Institutional Review Board. The questionnaire was distributed via email as a Survey Monkey link to all Accreditation Council for Graduate Medical Education (ACGME)-approved family medicine residency program directors in September 2019. Six follow-up emails were sent to encourage participation. Data collection closed after November 2019.
The baseline CERA questionnaire covered individual demographics (eg, gender, ethnicity, amount of time spent as program director at current program) and program demographics (eg, location, size of the program, approximate size of the community served). Vasectomy items in the questionnaire included time spent by residents learning about vasectomy, number of vasectomies performed during residency, program director views on vasectomy training, other specialties interest and/or involvement in training family medicine residents in vasectomies. Time spent learning about vasectomy was approximated by summing the number of hours spent in didactics and receiving clinical experience, such that a resident with two 1-hour didactic/simulation sessions plus one-half day in vasectomy clinic would sum to 6 hours or <1 day. A faculty champion was defined as someone who demonstrates commitment, advocacy, or advanced skills in vasectomy. The number of vasectomies performed during residency was categorized as none, only simulated, 1-2, 3-5, 6-10, and more than 10. Our main outcome was resident performance of more than five vasectomies before graduation. Individual and program characteristics, as well as vasectomy-education items, were examined as potential factors influencing the performance of more than five vasectomies during residency.
We tabulated the frequencies of all predictor variables and the main outcome variable to describe our respondent sample and the landscape of vasectomy training. We used χ2 tests, and Fisher’s exact tests where appropriate, to explore associations between the categorical predictor variables and the primary outcome of more than five vasectomies per graduating resident. We used logistic regression to predict the outcome of more than five vasectomies completed during residency. All statistical analyses were conducted using Stata Statistical Software, release 16 (StatCorp., College Station, TX).
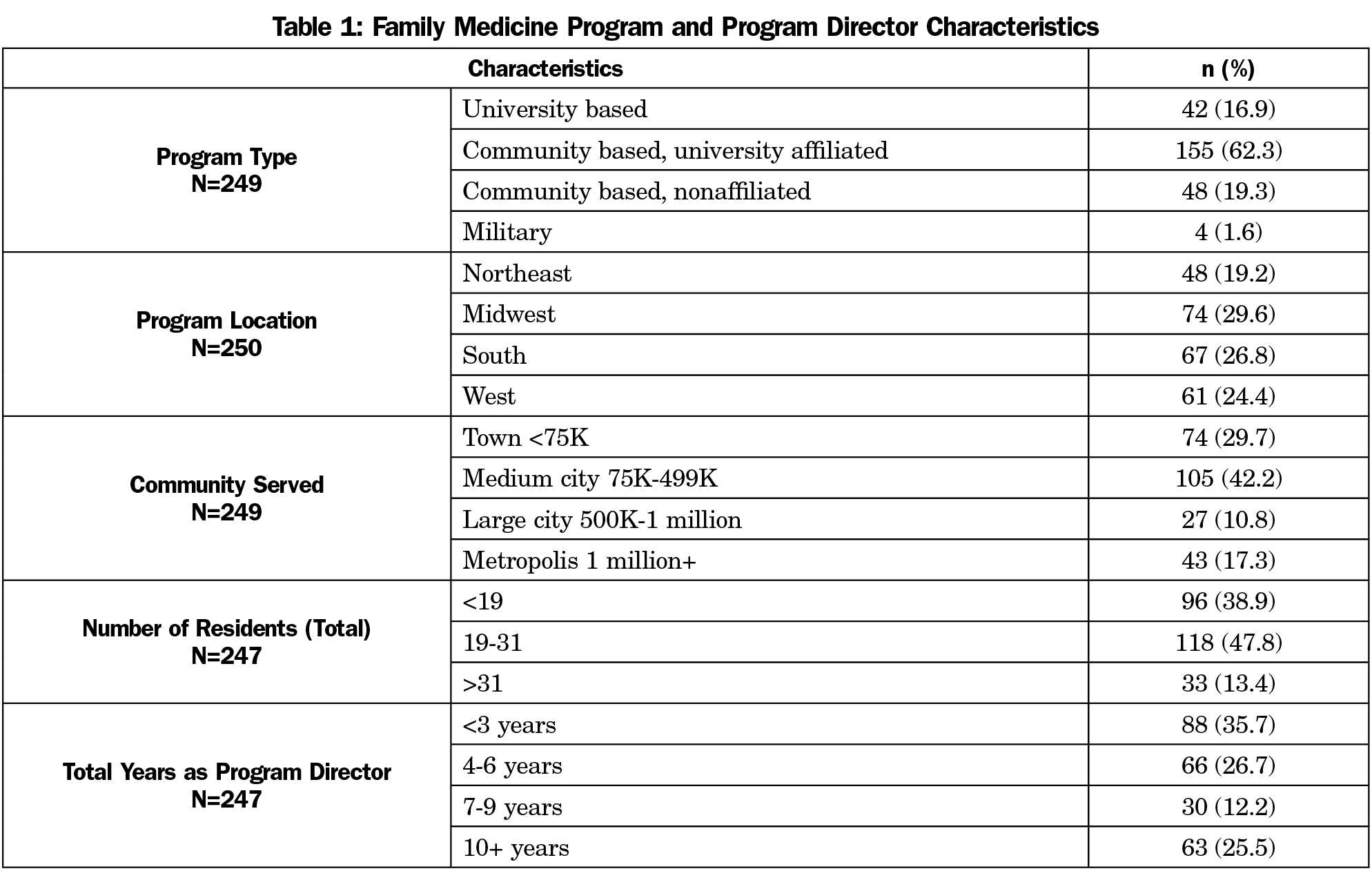
Of 628 surveyed residency program directors, we received 250 responses (response rate=39.8%). Respondents represented programs across all regions of the country, serving the full range of community sizes, with the majority serving populations of less than 500,000 (71.9%). Almost half of the programs had between 19-31 residents (47.8%) total (Table 1).
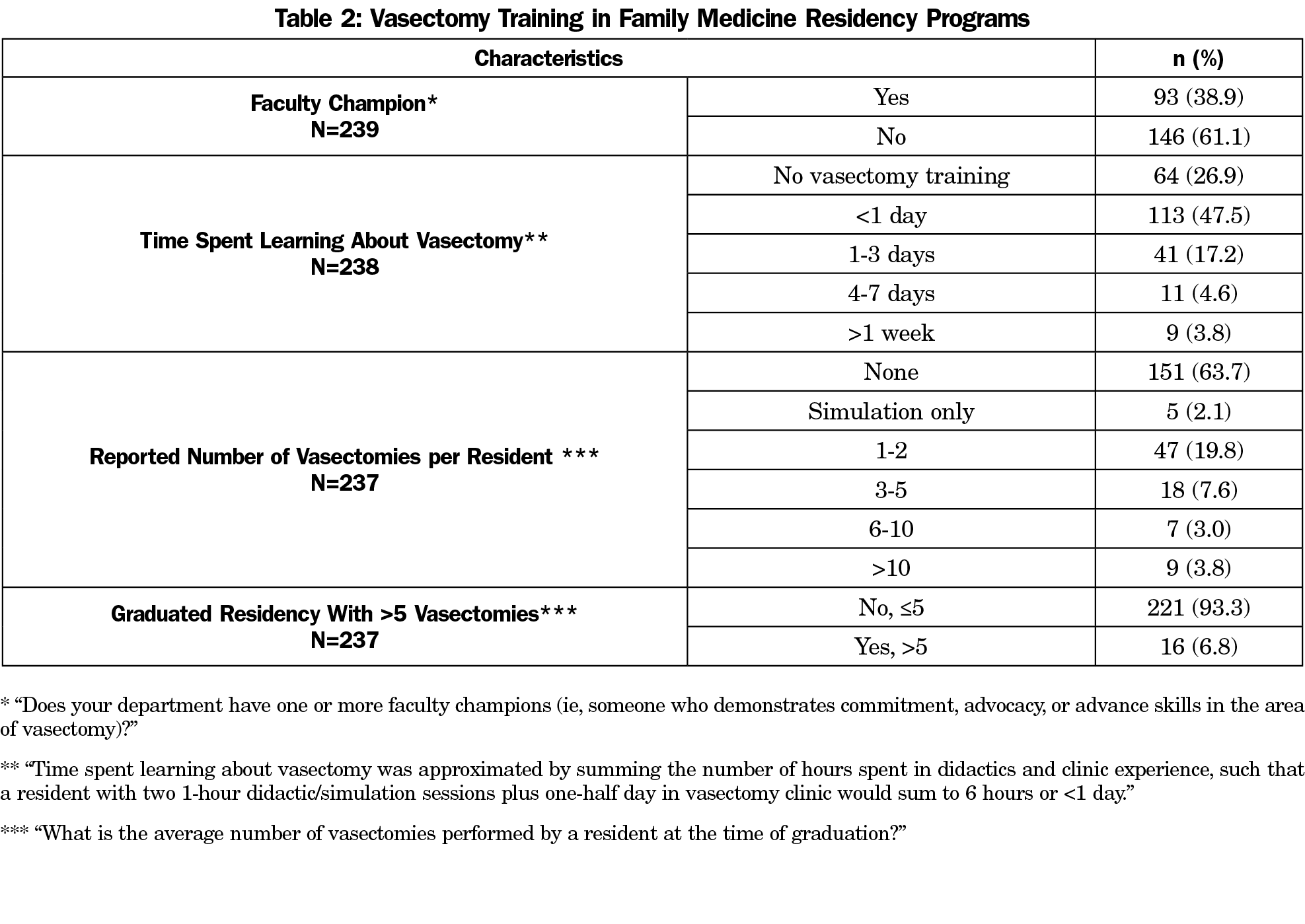
Table 2 shows the amount of time spent by residents on average over their entire residency learning about vasectomy care, which may have included didactics on preoperative counseling and evaluation, vasectomy procedure, postoperative care, and complications. Nearly three-quarters (73.1%) of programs offered vasectomy didactics and/or procedural training. Approximately half (47.5%) of programs had less than 1 day of vasectomy didactics and/or procedural training; 8.4% of programs spent more than 3 days teaching about vasectomy. A faculty champion was reported at 38.9% of programs. Residents on average graduated having performed more than five vasectomies in 6.8% of programs surveyed.
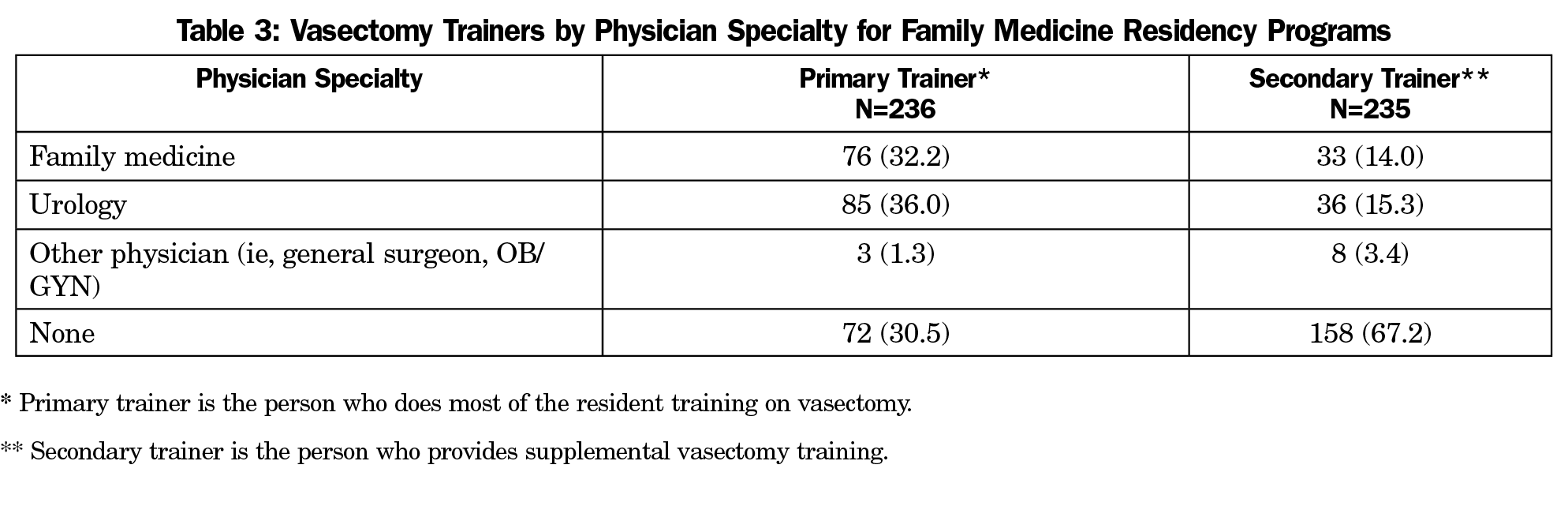
Nearly one-third (30.5%) of residency programs did not have a primary vasectomy trainer for their residents. As seen in Table 3, residents received vasectomy training from family medicine and urology faculty at similar rates (primary training: 32.2% vs 36.0%, secondary training: 14.0% vs 15.3%, respectively) General surgeons and obstetricians/gynecologists accounted for only 1.3% and 3.4% of primary and secondary trainers. Almost three-quarters (74.3%) of residency program directors believed their residents do not expect or intend to provide vasectomy to their patients after graduation; 4.2% of program directors reported that family medicine physicians should not be performing vasectomies. Approximately three-quarters (75.6%) of program directors report difficulty providing interested residents with enough training opportunities. Nearly a quarter (22.8%) of program directors reported meeting resistance with other specialties when trying to form partnerships to expand vasectomy training for their residents.
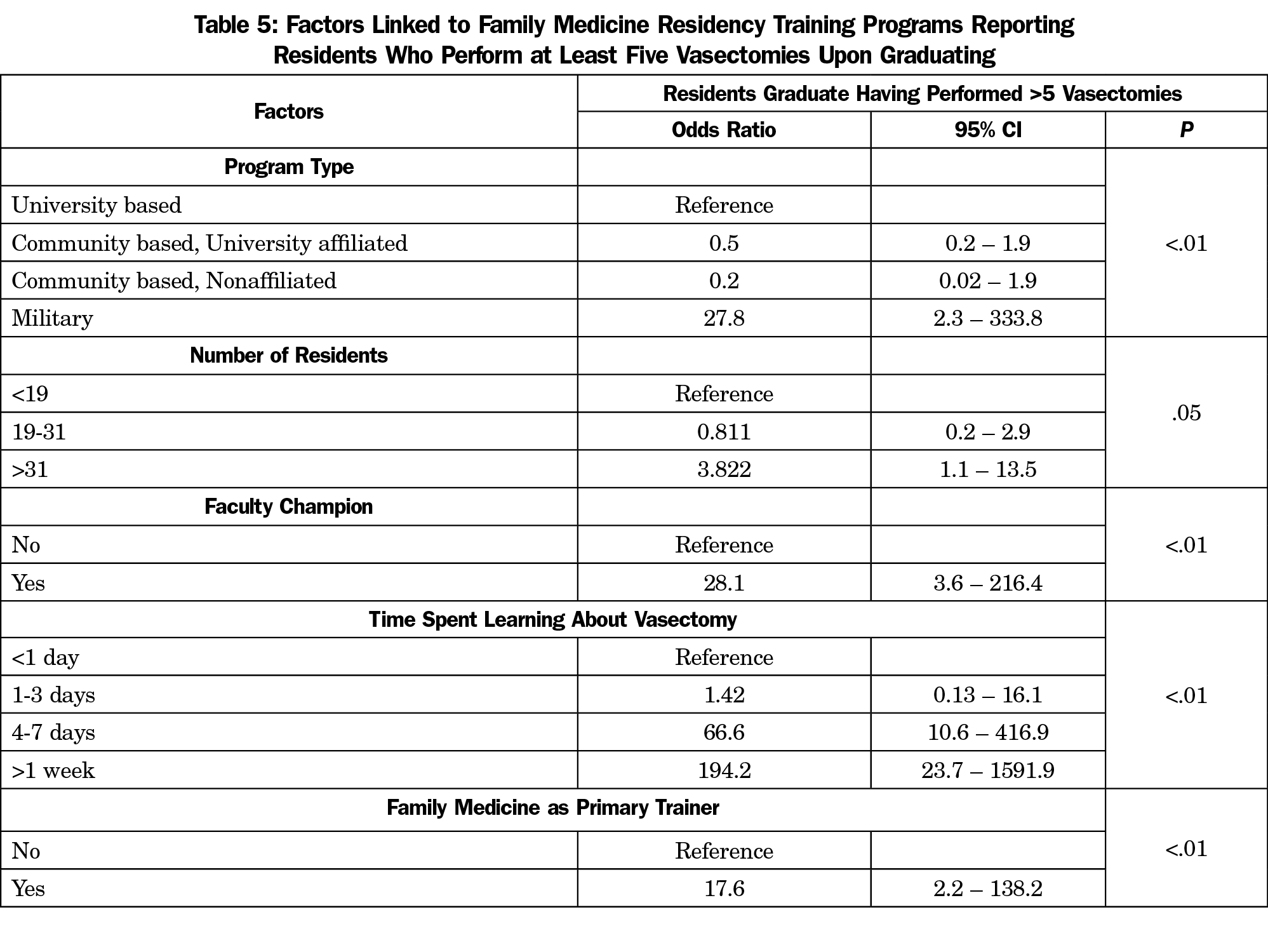
Table 4 examines factors associated with programs graduating residents with more than five vasectomies performed on average. Factors significantly associated with this outcome included (P<.05): program type, number of residents, time spent learning about vasectomy, having a faculty champion, and family medicine faculty serving as primary trainers. Program location, size of the community served, total years as program director, or urologists as primary or secondary vasectomy trainers were not significantly linked to the outcome. Table 5 reviews the unadjusted odds ratios for our significant predictors. Having a vasectomy faculty champion (OR 28.1, CI 3.6-216.4), family medicine faculty as primary vasectomy trainers (OR 17.6, CI 2.2-138.2), and increased time spent learning about vasectomy (4-7 days OR 66.6, CI 10.6-416.9; >1 week OR 194.2, CI 23.7-1,591.9) were the variables that significantly increased the odds of graduating residents who performed more than five vasectomies on average. We were unable to perform adjusted multivariate logistic regression due to the small cell sample sizes.
While the CAFM 2009 Consensus Guidelines for procedural training expect all residents to be exposed to and have the opportunity to train for independent performance in vasectomy,10 vasectomy training opportunities have continued to decline across family medicine residency programs since 2011. Our data show that only 6.8% of programs surveyed have residents who, on average, graduates having performed more than five vasectomies during their residency, the minimum requirement for procedural competence as outlined in a CAFM consensus statement. Compared to 1989 when 22% of programs graduated residents who had performed more than 10 vasectomies,5 only 3.8% of current family medicine program directors currently report more than 10 vasectomies by a resident on average. However, the rates of any vasectomy didactic or procedural training are similar to previous reports from 2011, with currently 73.1% of residency programs offering any training compared to 75.3% offering didactics and 72.1% offering clinical experience in 2011.7 Nonetheless, our data show that 47.5% of residency programs spend less than 1 day on vasectomy training. Given family physicians serve as an access point for men to discuss their reproductive goals and how to achieve them,12 adequate training on vasectomy is integral to their facilitating comprehensive men’s health.
Programs with the highest success in graduating residents with vasectomy experience had a faculty champion committed to vasectomy provision and training. We found champions across 38.9% of programs, noting as well that programs containing champions were significantly more likely to graduate residents performing more than five vasectomies per year. This finding is not particularly surprising, as a 2017 study evaluating an intervention designed to increase residents’ experience in reproductive health training through faculty advocates led to an increase in residents’ experience in procedures such as IUD insertion (from 85% to 99%) and contraceptive implant insertion (60% to 85%).13 Likewise, we found that when a program’s primary vasectomy trainer was a family physician, the program’s residents were more likely than those with vasectomy trainers from other specialties to graduate residents with more vasectomy procedural experience.
Furthermore, the lack of vasectomy training in residency may reflect program directors’ belief that residents are not interested in the skill; 74.3% of our residency program director respondents believed their residents do not expect or intend to provide vasectomy to their patients after graduation. However, a lack of data exists on resident interest in vasectomy provision. Some (4.2%) program directors even believe that family physicians should not be performing vasectomies, which may influence their offering of training opportunities for residents. Additionally, 75.6% of program directors cited a lack of adequate training opportunities for their residents despite collaborations with urologists, who were the primary trainers for 36.0% of programs. Interestingly, urology residents also cite a lack of volume as a reason for their discomfort with vasectomy as an in-office procedure.14 Given urologists also need to provide training opportunities for urology residents, it is not surprising that 22.8% of responding program directors have met resistance from other specialties when trying to form partnerships to expand vasectomy training.
This study is limited by our lack of data on nonresponding programs. However, we have no reason to believe their vasectomy training is much different and may even be less such that our findings may overestimate the prevalence of training, which would be more concerning. Further, our limited sample size prevents us from conducting reliable regressions that might better control for interactions and confounding among individual and program-related factors influencing vasectomy training at the programs. Lastly, barriers for resident patients to receive vasectomy, such as insurance coverage, were not addressed in this study.
Our data show that the majority of family medicine residency programs are not able to provide the resident on average with the minimum number of vasectomies deemed necessary for competency and independent provision before graduation. Without this necessary training, future family physicians will not be able to offer this important permanent contraceptive method to their patients and maintain a broad scope of practice. We found that a faculty champion or family medicine faculty who perform vasectomies may be able to inspire and train others to ensure continuation of vasectomy services.
Acknowledgments
Financial Disclosure: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Author D.M.H. was supported by grants from NIH (UL1TR002240 and P30CA046592).
References
- Shih G, Turok DK, Parker WJ. Vasectomy: the other (better) form of sterilization. Contraception. 2011;83(4):310-315. Accessed June 28, 2019. doi:10.1016/j.contraception.2010.08.019
- Contraceptive Use in the United States. Guttmacher Institute. https://www.guttmacher.org/fact-sheet/contraceptive-use-united-states#
- Ross JA. Engender Health. Male sterilization. In: Contraceptive Sterilisation: Global Issues and Trends. New York: EngenderHealth; 2002. p. 24–32.
- Barone MA, Hutchinson PL, Johnson CH, Hsia J, Wheeler J. Vasectomy in the United States, 2002. J Urol. 2006;176(1):232-236. doi:10.1016/S0022-5347(06)00507-6
- Denniston GC, Eggertsen SC. A national survey of vasectomy training in family practice residency programs. Fam Med. 1989;21(5):384-386.
- Sharp LK, Wang R, Lipsky MS. Perception of competency to perform procedures and future practice intent: a national survey of family practice residents. Acad Med. 2003;78(9):926-932. Accessed June 28, 2019. doi:10.1097/00001888-200309000-00019
- Herbitter C, Greenberg M, Fletcher J, Query C, Dalby J, Gold M. Family planning training in US family medicine residencies. Fam Med. 2011;43(8):574-581.
- CAFM Consensus Statement for Procedural Training in Family Medicine Residency. Council of Academic Family Medicine. Accessed May 9, 2022. https://www.afmrd.org/page/cafm
- Mainous AG III, Seehusen D, Shokar N. CAFM Educational Research Alliance (CERA) 2011 Residency Director survey: background, methods, and respondent characteristics. Fam Med. 2012;44(10):691-693. Accessed March 17, 2021. https://europepmc.org/article/med/23147999
- Nothnagle M, Sicilia JM, Forman S, Fish J, Ellert W, Gebhard R, Kelly BF, Pfenninger JL, Tuggy M, Rodney WM; STFM Group on Hospital Medicine and Procedural Training. Required procedural training in family medicine residency: a consensus statement. Fam Med. 2008 Apr;40(4):248-52.
- Haws J, McKenzie M, Mehta M, Pollack A. Increasing the availability of vasectomy in public-sector clinics. Guttmacher Institute. Family Planning Perpectives. 1997. 29(4):185-186). Accessed May 9, 2022. https://www.guttmacher.org/journals/psrh/1997/07/increasing-availability-vasectomy-public-sector-clinics
- Jones HE, Calixte C, Manze M, et al. Primary care patients’ preferences for reproductive health service needs assessment and service availability in New York Federally Qualified Health Centers. Contraception. 2020;101(4):226-230. doi:10.1016/j.contraception.2019.12.003
- Aleza K. Summit, MPH; Marji Gold M. The effects of abortion training on family medicine residents’ clinical experience. Fam Med. 2017;49(1):22-27.
- Wagner KE, Soyster ME, Bartels C, Honig S, Harnisch BA. Improving resident learning on vasectomy: a national survey on urology resident vasectomy training. Can J Urol. 2021;28(6):10941-10945.




There are no comments for this article.