Background and Objectives: There is limited data on primary care physicians (PCPs) who suffered from COVID-19. We aimed to assess the proportion of PCPs with COVID-19, the proportion hospitalized with COVID-19, and the number of days off work. We also explored their psychological suffering due to the pandemic.
Methods: We selected a random sample of 1,000 PCPs practicing in the seven cantons of Western Switzerland (November/December 2020). PCPs were invited by mail to complete a questionnaire.
Results: The participation rate was 51% (N=506). The burden of disease was high among PCPs: 13% suffered from COVID-19, 0.4% needed hospitalization, and 10 days off work were required on average. In addition, many PCPs reported experiencing heightened psychological symptoms, mainly fatigue (53%) and stress/anxiety (48%).
Conclusions: These findings highlight the urgent need to implement preventive measures to reduce the risk of COVID-19 and psychological illness in PCPs.
Primary care physicians (PCPs) have been on the front line from the beginning of the pandemic to care for COVID-19 patients. However, to our knowledge, there are no data on the number of PCPs who suffered from symptomatic COVID-19. According to seroprevalence studies, they do not appear to be a high-risk population.1,2 In contrast, it was shown that they frequently suffer from psychological disorders related to the pandemic and isolation due to national lockdowns, such as burnout,3 generalized anxiety4 and stress.5
We aimed to quantify the proportion of Swiss PCPs who suffered from symptomatic COVID-19 and to assess the medical (hospitalizations) and professional (sick leave) consequences of COVID-19. We also explored the psychological suffering of PCPs related to the pandemic.
Study Site and Study Population
For this cross-sectional study conducted in November/December 2020, we selected a nonstratified random sample of 1,000 physicians from a list of all 2,455 PCPs practicing in the seven cantons of Western Switzerland (men=53.4%; general practitioners [GPs]=69.0%, pediatricians=17.5%, gynecologists=13.5%).
Data Collection
PCPs were invited by mail to complete an anonymous questionnaire with sociodemographic items (gender, age group, medical specialty, type and location of practice, number of half-days worked per week) and questions related to COVID-19 (symptomatic SARS-CoV-2 infection confirmed by RT-PCR test [Y/N], number of days of hospitalization, number of days off work). They were also asked if they had experienced psychological symptoms (five items: stress and/or anxiety, sleep disorders, depression symptoms, burnout symptoms, fatigue) more intensively than usual due to the pandemic and lockdown measures (Y/N). Reminder messages (one per physician) were sent to nonresponders. There was no financial compensation for participation. The questionnaire was pretested by five PCPs to identify difficulties in responding to the questions, and adapted after their suggestions.
Confidentiality and Ethical Approval
All data were collected in an anonymous manner. Informed consent was obtained from all participants included in the study. The study was approved by the Cantonal Commission for Research Ethics (number: 2019-01850).
Statistical Analyses and Sample Size
We used frequency tables to describe categorical variables, and medians and interquartile ranges to summarize discrete numerical variables. We investigated associations with sociodemographic factors using χ2 tests and Wilcoxon-rank sum tests. For the variables that were statistically significantly associated with sociodemographic factors at a P value ≤.05, we carried out multivariable logistic regressions, adjusting for gender, age group and medical specialty.
We calculated the sample size to estimate the proportion of 50% (the proportion with the largest sample size), with a 95% confidence interval width of 0.10 (10%) around the estimate. The minimal sample size required for the study was 385. Given the expected 40% participation rate, 1,000 physicians were invited to participate. We performed all statistical analyses with STATA 15.1 software (STATA Corp, College Station, TX).
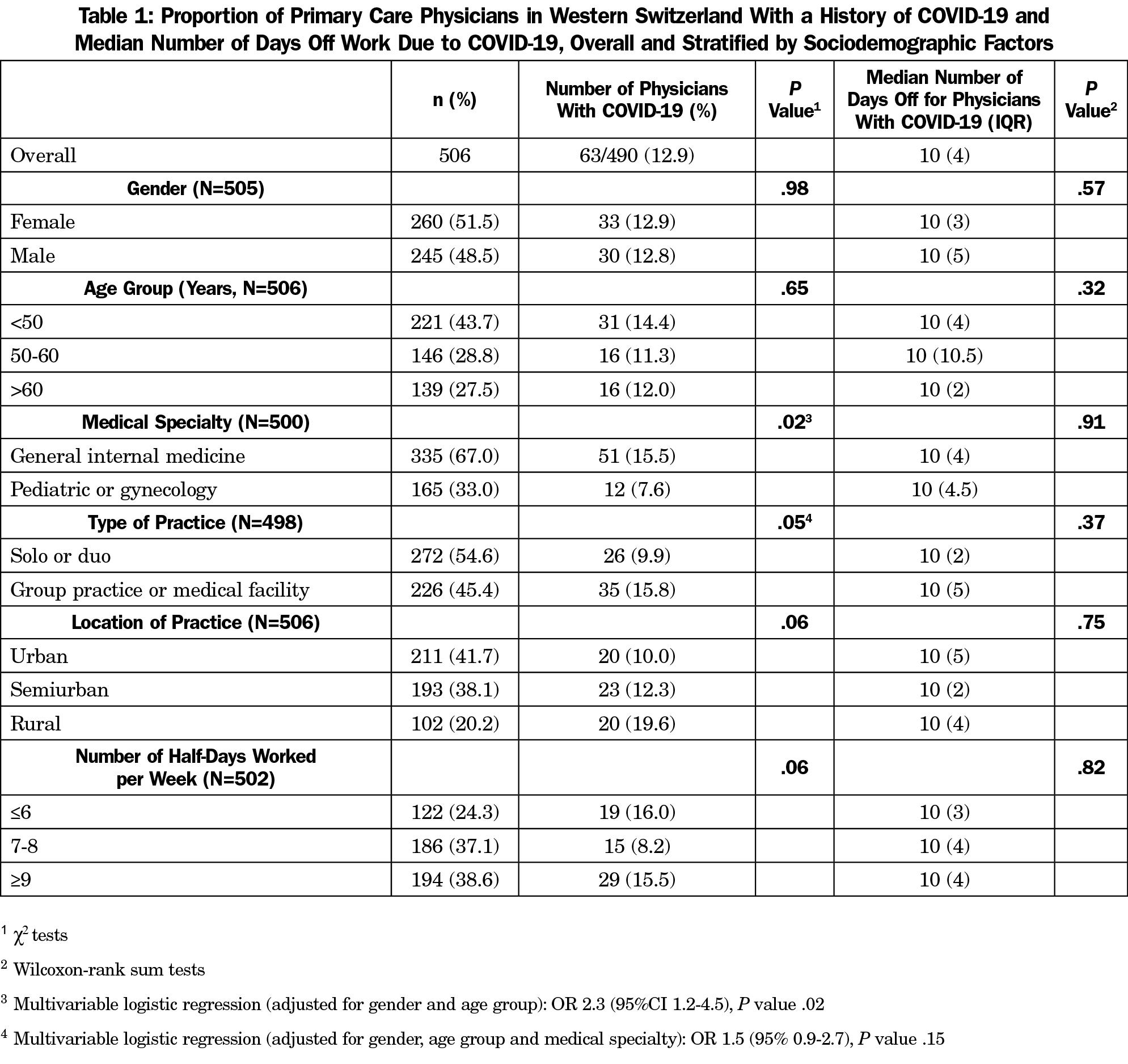
Of the 1,000 PCPs contacted, 506 agreed to participate (51% participation rate). Fifty-two percent were women; 56% were over 50 years of age; two-thirds were GPs and one-third were pediatricians or gynecologists (Table 1). Compared to the list of 2,455 PCPs practicing in Western Switzerland, the study sample was comparable regarding gender and medical specialty (men=53.4% vs 48.5%; GPs=69.0% vs 67%, pediatricians and gynecologists=31.0% vs 33.0%).
Overall, 63 PCPs (13%) had a symptomatic SARS-CoV-2 infection confirmed by RT-PCR test. The proportion of physicians with COVID-19 was higher among GPs (16% versus 8%, adjusted OR=2.3 [95%CI 1.2-4.5], P=.02). Two physicians (one GP, one pediatrician) were hospitalized for COVID-19. The median number of days of sick leave was 10 (IQR=4, max=35), with no statistically significant difference between the subgroups.
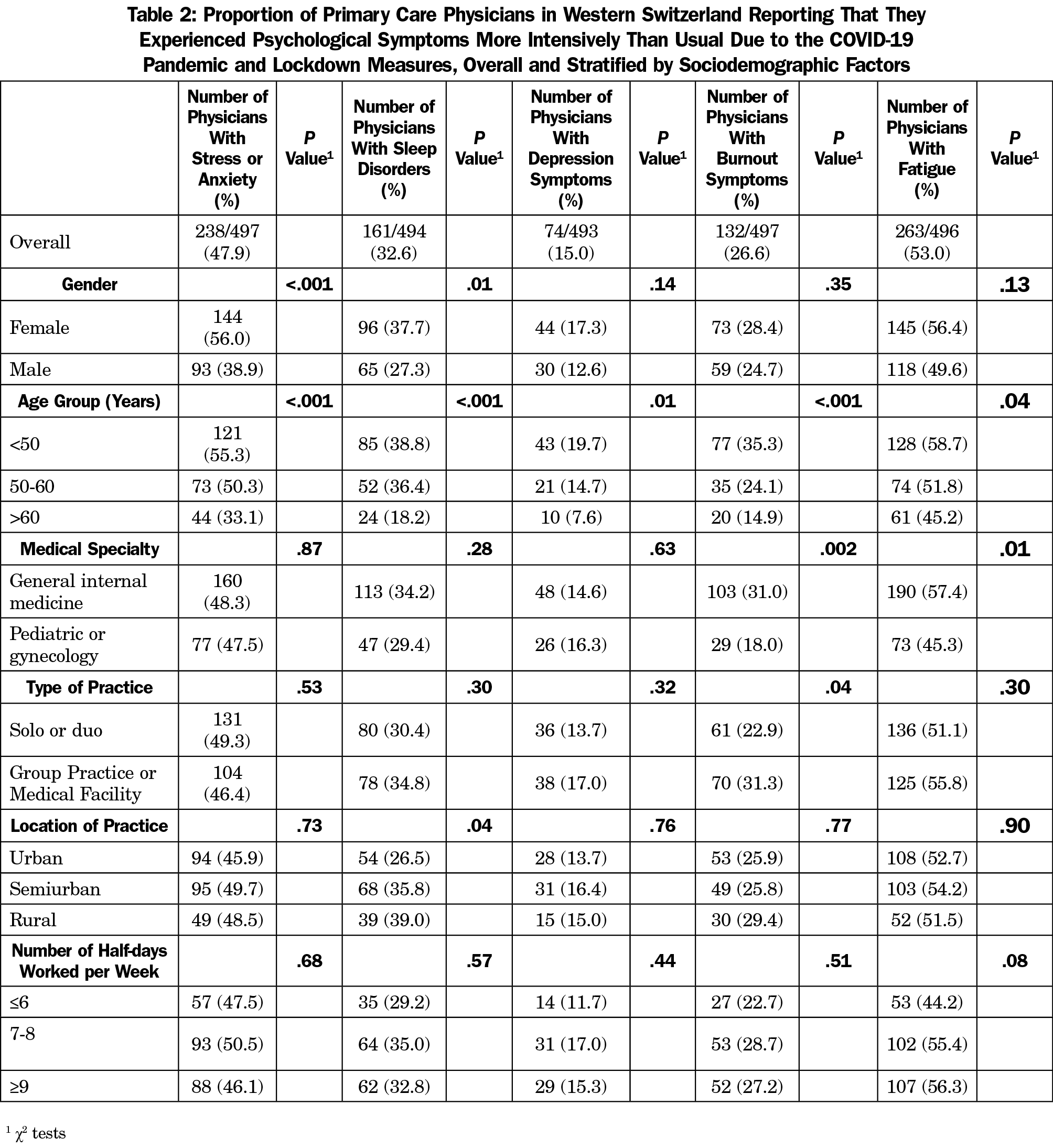
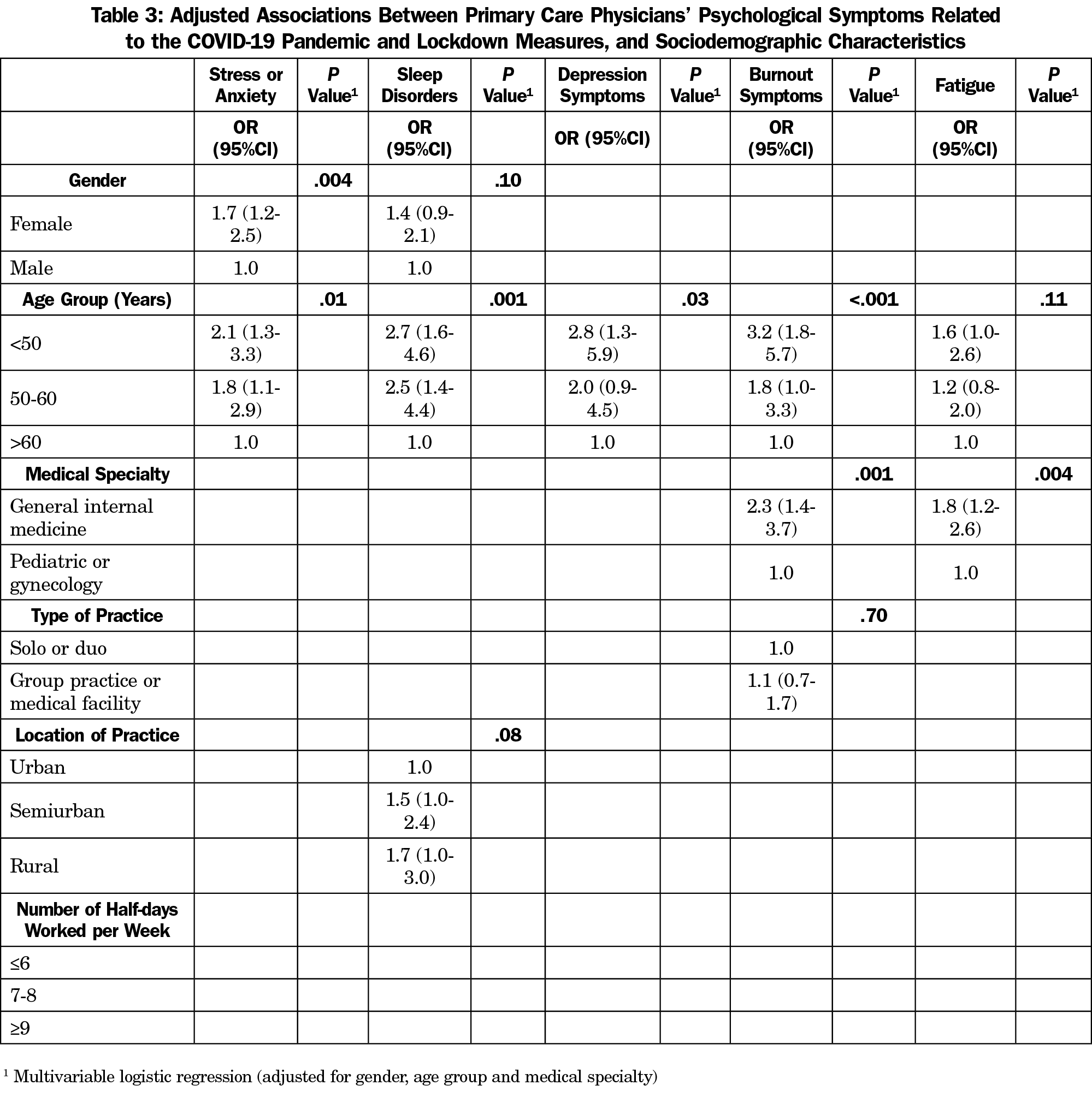
Many physicians reported experiencing psychological symptoms more intensively than usual due to the pandemic (Table 2), mainly fatigue (53%) and stress/anxiety (48%). In multivariable analysis, GPs (for burnout symptoms and fatigue), younger physicians (for all symptoms) and female physicians (for stress/anxiety) tended to suffer from psychological symptoms more often than pediatricians/gynecologists, older, and male physicians, respectively (Table 3).
Main Findings
The burden of disease was high among PCPs: 13% suffered from COVID-19, 0.4% needed hospitalization, and 10 days off work were required on average. Many PCPs reported experiencing heightened psychological symptoms, mainly fatigue (53%) and stress/anxiety (48%).
Comparison With Existing Literature
The proportion of PCPs with COVID-19 was about two times higher than that of the general population living in Western Switzerland (COVID-19 rate until November 2020=6% and until December 2020=7%). Our results, focusing on symptomatic infections, contradict seroprevalence studies that concluded that PCPs had a relatively low risk of infection.1,2
Several studies highlighted the psychological suffering experienced by PCPs.3–5 Our study confirms these findings. This suffering can be related to the stress experienced when treating COVID-19 patients, where emotions can overwhelm coping capacities.3 We found that GPs, younger and female physicians were particularly at risk. A systematic review also showed that young and female health care workers were particularly at risk of developing psychological symptoms.6
At the time of the study, COVID-19 vaccines were not yet available. Switzerland’s overall strategy to manage the epidemic is currently based on three pillars: vaccinations, testing, and nonpharmaceutical measures. The Swiss Federal Council developed a three-phase model outlining the strategic approach until the end of the COVID-19 crisis, focusing on increasing vaccination coverage and recommending large-scale, repetitive testing.7 The majority of the population supports the Federal Council’s strategy. However, as in other countries, demonstrations and civil unrest related to the prevention strategies put increasing pressure on policy makers. The involvement of PCPs in the pandemic is highly variable in Switzerland due to the liberal organization of the health care system. For example, a number of PCPs do not test patients with suspected COVID-19 in their offices.
Strengths and Limitations
Our study had a high response rate, but has some limitations. It was solely conducted in Switzerland; the results are not necessarily representative of other countries. Indeed, SARS-CoV-2 infection rates and government measures to fight the pandemic vary considerably between countries. In addition, the results of the study are based on self-reported data; a certain percentage of incorrect data cannot be excluded, especially for questions related to psychological symptoms.
More preventive measures to reduce the risk of SARS-CoV-2 infection and psychological illness in PCPs are urgently needed, since PCPs are in the front line of providing care to populations during the pandemic.
Acknowledgments
The authors thank all the physicians who agreed to participate in this study.
References
- Ledda C, Carrasi F, Longombardo MT, Paravizzini G, Rapisarda V. SARS-CoV-2 seroprevalence post-first wave among primary care physicians in Catania (Italy). Trop Med Infect Dis. 2021;6(1):21. doi:10.3390/tropicalmed6010021
- Martín V, Fernández-Villa T, Lamuedra Gil de Gomez M, et al. Prevalence of SARS-CoV-2 infection in general practitioners and nurses in primary care and nursing homes in the healthcare area of León and associated factors. Semergen. 2020;46(suppl 1):35-39. doi:10.1016/j.semerg.2020.05.014
- Di Monte C, Monaco S, Mariani R, Di Trani M. From resilience to burnout: psychological features of Italian general practitioners during COVID-19 emergency. Front Psychol. 2020;11:567201. doi:10.3389/fpsyg.2020.567201
- Monterrosa-Castro A, Redondo-Mendoza V, Mercado-Lara M. Psychosocial factors associated with symptoms of generalized anxiety disorder in general practitioners during the COVID-19 pandemic. J Investig Med. 2020;68(7):1228-1234. doi:10.1136/jim-2020-001456
- Dutour M, Kirchhoff A, Janssen C, et al. Family medicine practitioners’ stress during the COVID-19 pandemic: a cross-sectional survey. BMC Fam Pract. 2021;22(1):36. doi:10.1186/s12875-021-01382-3
- d’Ettorre G, Ceccarelli G, Santinelli L, et al. Post-traumatic stress symptoms in healthcare workers dealing with the COVID-19 pandemic: a systematic review. Int J Environ Res Public Health. 2021;18(2):E601. doi:10.3390/ijerph18020601
- Coronavirus: Situation in Switzerland [Internet]. Switzerland Federal Office of Public Health. Accessed November 28, 2021. https://www.bag.admin.ch/bag/en/home/krankheiten/ausbrueche-epidemien-pandemien/aktuelle-ausbrueche-epidemien/novel-cov/situation-schweiz-und-international.html



There are no comments for this article.