Background and Objectives: Public health training became particularly important for family medicine (FM) residency training programs amid the COVID-19 pandemic; the Accreditation Council for Graduate Medical Education (ACGME IV.C.19) requires a structured curriculum in which residents address population health. Our primary goal was to understand if, and to what extent, public health interventions trainings were incorporated into FM residency training programs amid the COVID-19 pandemic. We hypothesized programs with more resources (eg, university affiliates) would be better able to incorporate the training compared to those without such resources (ie, nonuniversity affiliates).
Methods: In 2021, we incorporated items addressing COVID-19 public health training competencies into the 2021 Council of Academic Family Medicine Educational Research Alliance national survey of FM residency program directors. The items addressed the type of training provided, mode of delivery, barriers to providing training, perceived importance of training, and support in delivering training.
Results: The overall survey response rate was 46.4% (n=287/619). All programs offered at least some training to residents. There were no statistically significant differences in training intensity between university and nonuniversity affiliates. The length of time an FM residency director spent in their position was positively associated with training intensity (r=0.1430, P=.0252). The biggest barrier to providing the trainings was the need to devote time to other curriculum requirements.
Conclusions: FM residency programs were able to provide some public health interventions training during the pandemic. With increased support and resources, FM resident training curricula may better prepare FM residents now in anticipation of a future pandemic.
The COVID-19 pandemic laid bare the importance of family medicine (FM) and public health, as well as the inadequacies in the United States’ current approach to primary care and public health. Physicians need knowledge and skills relevant to contact tracing, and effective communication around testing, quarantine, vaccination, and community outreach.
A study by the Centers for Disease Control and Prevention (CDC) found that 35% to 48% of patients with COVID-19 did not report their close contacts when contacted by the local health department. They postulated this may have been attributed to the lack of connection and trust between the local health department and patients.1 In a study by Staes et al, most health care professionals (HCP) in an urgent care setting were able to correctly identify the health department’s role in contact tracing.2 Therefore, FM may be able to bridge the connection, given its strong ties to and rapport with patients and the community.3-5
The Accreditation Council for Graduate Medical Education (ACGME IV.C.19) requires a structured curriculum in which FM residents address population health.6 Although the ACGME has a requirement for population health and not public health, there is a unique integration of both in FM. This integration has been highlighted during the COVID-19 pandemic. For example, some providers have been called to manage COVID-19 symptoms among their patient panel and inform return-to-school policies for children in their community.7 Cancer screening is another example of a public health effort that has been successfully managed by primary care providers during the pandemic.8
COVID-19 is still spreading, and it is not likely be the last pandemic FM clinicians will face during their careers.9 The essential lessons drawn from the intersection of the rapidly-changing COVID-19 pandemic, public health interventions, and FM training can be used to enhance training curricula, keep patients safe, and to improve public health and the primary care system. Currently, scientific knowledge is lacking on how COVID-19 may have affected FM residency training curricula around public health. Thus, there is a need to understand how and if public health interventions were incorporated into FM residency training programs amid the COVID-19 pandemic.10
To address this gap we surveyed FM program directors to provide a national snapshot. We hypothesized FM residency programs with a university affiliation would have more resources and capacity to train their residents in public health intervention during the COVID-19 pandemic compared to those without an affiliation.
Sample
Our survey was included in the 2021 Council of Academic Family Medicine Educational Research Alliance (CERA) national FM residency Program Directors Survey. CERA is a joint initiative of four major US academic FM organizations including the Society of Teachers of Family Medicine, North American Primary Care Research Group, Association of Departments of Family Medicine, and the Association of Family Medicine Residency Directors. FM residency program directors that are members of at least one of the four academic FM organizations and had at least three resident classes were eligible to participate. The methodology of the CERA Program Director Survey has previously been described in detail.11
The survey invitation was emailed to 619 eligible FM residency program directors using SurveyMonkey software. After the initial invitation, four follow-up emails were sent to encourage nonresponders to complete the survey. The data were collected from April 14, 2017 to May 17, 2021.
The American Academy of Family Physicians Institutional Review Board approved the project.
Survey Items
The survey included background questions on FM residency program director demographics, their departmental characteristics, and public health training provided to residents relevant to the COVID-19 pandemic. We used previous reports on primary care’s role in the pandemic as a guiding framework to develop the public health training questions.12,13 We selected four training domains related to COVID-19 training: resources, policies, guidelines, and communication. We asked directors about the type and mode of delivery (didactic, experiential, both), barriers to providing the training, importance of training, and support in delivering training. Examples included “How did you provide [contact-tracing guidelines] training to your FM residents during the COVID-19 pandemic?” and “What was the biggest barrier to providing these trainings?” The response options included a matrix and Likert scales (see Appendix).
The CERA Steering Committee evaluated questions for consistency with the overall subproject aim, readability, and existing evidence of reliability and validity. Pretesting was done with FM educators who were not part of the target population. Based on pretesting, we modified some questions for flow, timing and readability.
Training Intensity
The four training questions asked if training was provided to residents around (1) COVID-19 related resources (eg, testing guidelines and insurance coverage), (2) policies (eg, sick leave and return to work after exposure), (3) contact tracing guidelines (eg, how to identify contacts), and (4) health literacy (eg, strategies for explaining complex information). We scored each response based on whether a training was not delivered (score=0), delivered didactically (score=1), delivered experientially (score=2), or delivered both didactically and experientially (score=3). We subsequently created a composite training intensity score by combining the four questions. Composite scores ranged from 0 to 12.
Analyses
We used STATA 16 (Stata Corporation, and College Station, TX) for our data analyses. We performed descriptive analyses on the FM residency director demographics and program characteristics using frequencies and proportions, and numerical measurements with means and standard deviations.
We used a t test to compare the mean training intensity scores between university affiliated (university based and community based, university-affiliated programs) and nonuniversity-affiliated programs (community based, nonuniversity affiliated; military; other programs). Next, we estimated correlation coefficients to determine if FM program director demographics or program characteristics were associated with training intensity. We used a P value of <.05 to determine statistical significance on all analyses.
Survey Respondent Demographics and Program Characteristics
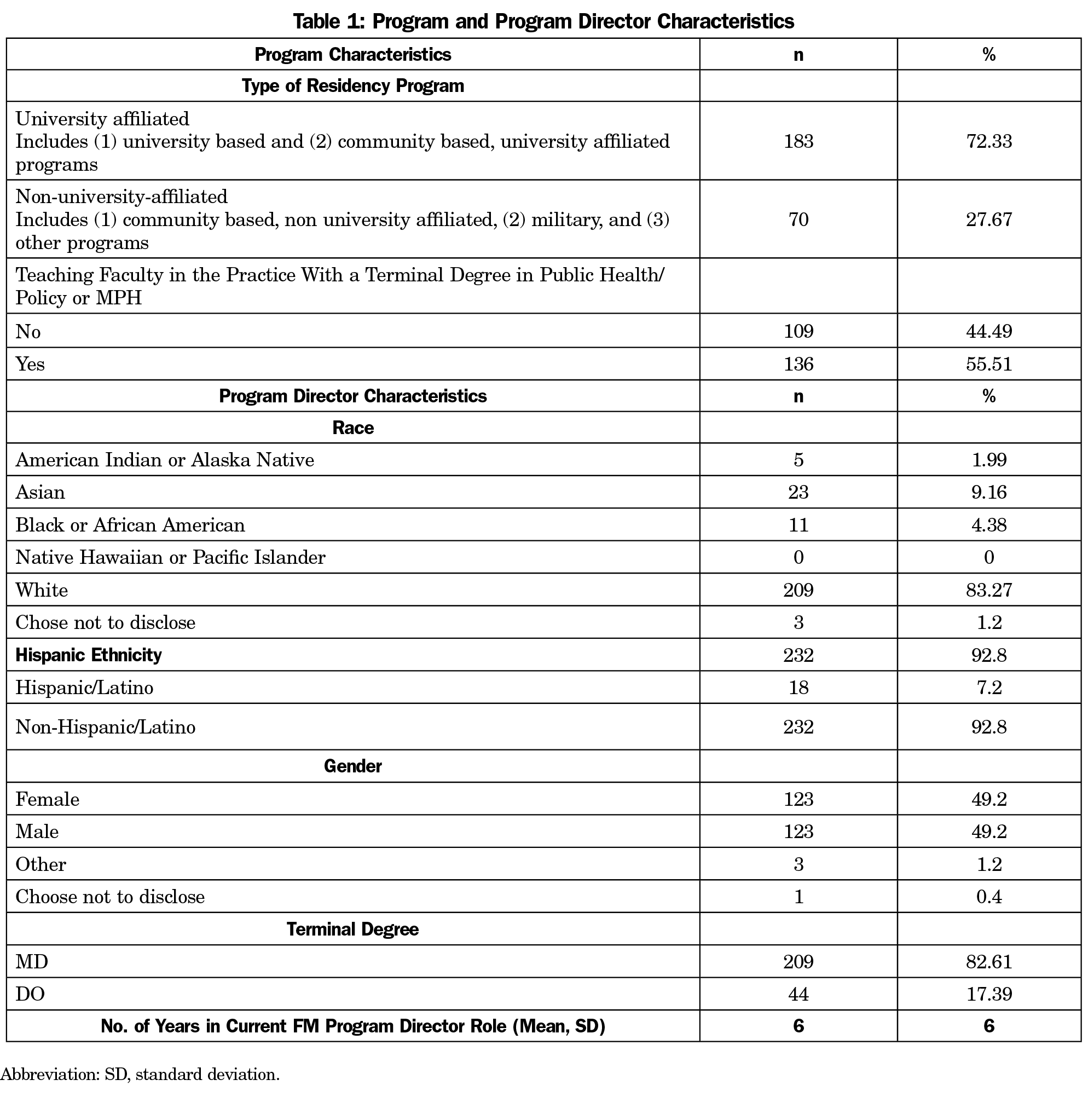
Two-hundred eighty-seven FM residency program directors completed our survey, for an overall survey response rate of 46.4%. Table 1 shows the descriptive data on FM residency directors and their programs. The FM residency program directors primarily identified as White, non-Hispanic and had spent a mean of 6 years in their role. Most programs were university affiliated (72.33%). More than half of the programs had teaching faculty with credentials in public health or health policy (55.5%).
Types of Trainings and Barriers to Delivery
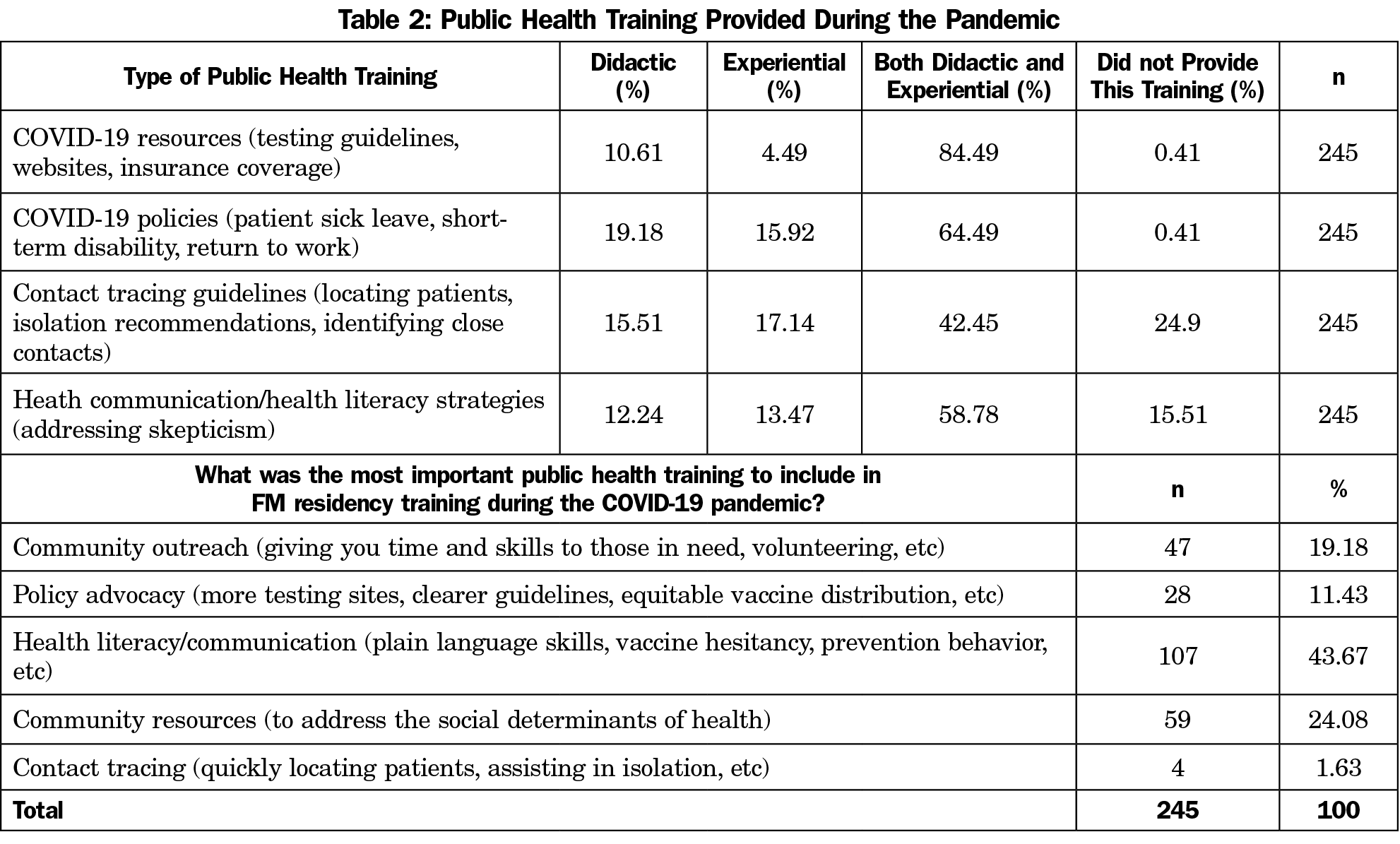
Most of the trainings were provided didactically and experientially, covering COVID-19 policies (99.6%) and resources (99.6%). Of all of the trainings, FM residency program directors indicated health literacy/communication was the most important during the pandemic (43.67%, Table 2). Very few felt there was no need to provide COVID-19 pandemic public health training (5.02%) or viewed it as a low priority (0.42%).
The majority of FM residency program directors indicated the biggest barrier to providing the trainings was the need to devote time to other curriculum requirements (61.51%, Figure 1). Other barriers included lack of needed resources and knowledge.
Training Intensity and Associations
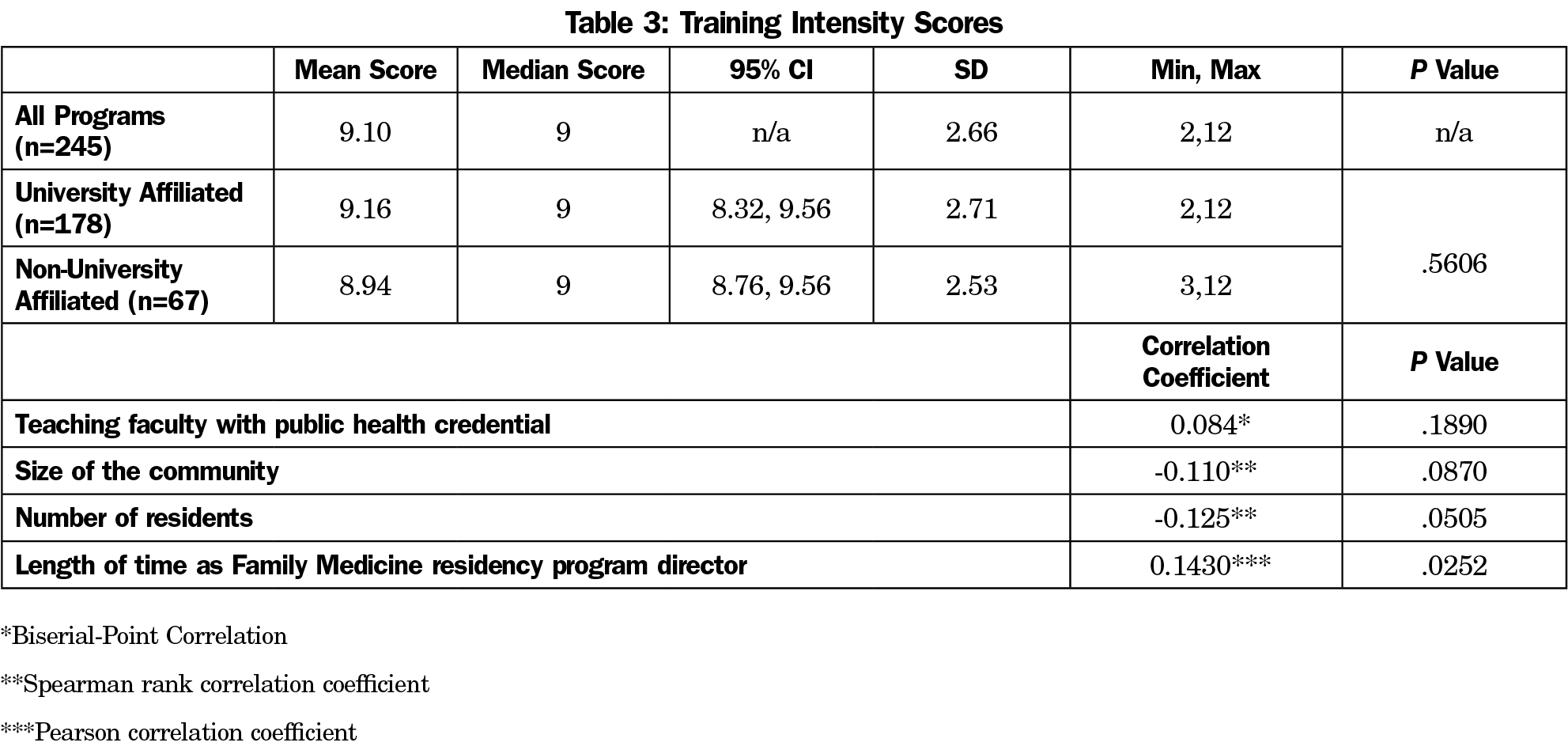
All of the programs indicated they were able to provide some training. The intensity of the training scores ranged from 2-12, with a median score of 9. There were no differences in mean scores between training intensity scores for university affiliated and nonuniversity-affiliated programs (9.16, 95% confidence interval [CI] 8.32-9.56 vs 8.94, 95% CI 8.76-9.56; P=.5606). Overall, 61% of the programs scored above or equal to the sample mean score of 9.10 (Figure 2). There was no statistically significant difference in the proportion of nonuniversity-affiliated practices and university-affiliated practices that scored above the mean (49.73%, CI 42.48-56.97 vs 57.47%, CI 47.08-67.86; P=.2338). Length of time as a FM residency director was the only characteristic associated with training score intensity (r=0.1430, P=.0252). Additional detail is available in Table 3.
Program directors responded to the COVID-19 pandemic by adapting their residency training to include COVID-19 resources and guidelines, policies, contact tracing, and communication skills. All of the programs offered some training, and none had a training intensity score of 0. More than half of all of the programs scored above the 50th percentile score (9), indicating most had an integrated (combined experiential and didactic) COVID-19 public health training program. These findings were independent of university affiliation, contrary to our hypothesis. Despite the challenges of delivering the curriculum and competing priorities, most FM programs offered a combination of didactic and experiential training in each of the training areas. These findings underscore the resilience of FM residency programs and their ability to adapt during a pandemic.
Despite the evidence that contact tracing represents a life-saving public health intervention,14 this was the most frequently reported training that was not provided (24.9%), and less than 2% of FM residency program directors saw it as an important training. Community-based contact tracing is provided by public health departments, while employee-based contact tracing often is done by the organization (eg, the hospital). The reasons a significant portion of programs did not offer training are not clear, but could reflect how the question was interpreted (ie, training in conducting contact tracing vs education regarding the processes).
Further, despite approximately 43.67% of FM residency directors endorsing health literacy and communications trainings as the most important topics for training during the pandemic, this training was the second most frequently reported as not provided (16%). These findings may indicate a need to close gaps in perceived need and support for FM residency programs to implement these trainings. We found a weak positive association between how long FM residency program directors spent in their role and training intensity in their programs. Quickly adapting FM residency curriculum in response to the pandemic represents a major leadership challenge. Potentially, longer tenure may reflect stronger leadership skills and reputational authority that facilitate implementation of these curricular changes.15 This may indicate a greater ability and or power to acquire training resources over time. These assertions will need to be explored in future studies.
Organizations such as the Accreditation Council for Graduate Medical Education should consider formally incorporating guidelines and resources around public health interventions training into curricula. This may include the need to allow FM residency program directors more autonomy in tailoring curriculum requirements during the time of a public health crisis and or providing tangible resources to help incorporate the trainings, as we found time (62%) and lack of resources (20%) were the biggest barriers. This is consistent with previous studies that have explored public health training in primary care settings.5,16 Future studies should explore the types and amounts of resources that programs need, as well as ideas on how time may be restructured and or redistributed. Based on the experience of the COVID-19 pandemic, FM residency program directors, faculty, and chairs should continue to ensure adequate training for FM residents and others in both public health pandemic preparedness, as well as evidence-based interventions in real time. Despite the early reports of a novel respiratory virus in Asia in December 2019, the US health care system was unprepared for the impact of the virus on the population and society. Early in the pandemic, health care leaders—including those in FM education—were rapidly reviewing and promulgating basic “nonpharmaceutical interventions” to avoid the spread of COVID-19.17 Given ongoing concerns about the changing climate and resultant shifts in infectious agents, the lived experience of practicing and teaching during this pandemic should remain a core activity in teaching future pandemic preparedness and intervention.
Our findings may also signal a need for incentivizing public health training in FM and making it more accessible. The Association of American Medical Colleges currently lists over 282 public health pathways for FM residents. Many of these programs are provided by organizations such as AcademyHealth, the Agency for Healthcare Research and Quality, and the American Association for the Advancement of Science.18 The programs tend to be formal fellowships of visiting scholar opportunities. Perhaps, given the already time intensive training for FM residents, there should be a shift toward developing self-paced programs that can be completed remotely from the residents’ home institutions. Additionally, the American Academy of Family Physicians may want to consider adding a certificate of added qualification (CAQ) in public health training, as public health training is currently not offered as a CAQ.19 A study found that family physicians with CAQs in sports medicine and geriatrics spent more of their time practicing in those respective areas within FM.20,21 Given this, a CAQ in public health may increase the workforce (ie, resources) around public health training in FM. This is important to consider, since only 55.5% of the FM residency program directors in our study reported they had a teaching faculty with a public health credential. Our recommendations are in line with a study by Morley et al that revealed the need for creative curricular solutions for providing public health training in FM outside the exam room.22
Limitations
Just under half of the FM program directors responded. It is plausible that programs offering little or no training were less likely to respond, thus overestimating training. The limited number of questions precluded exploration of reasons for not offering training in some areas. The cross-sectional design precludes causal inferences regarding the associations and direction of associations.23 Our survey was also self-report and our training score was a composite; therefore, our findings may not represent the actual frequency and intensity of training activities based on the number of hours. To our knowledge, our study is the first to examine FM residency training around COVID-19. As such, we developed our survey de novo, and we cannot speak to its reliability and validity. There may have been other questions or constructs that were important, but not captured in our survey.
This study demonstrates that FM residency programs adapted to the COVID-19 pandemic by delivering public health interventions training. Building on this knowledge, the provision of resources and support for programs to include their FM resident training curriculums now may better prepare FM residents in anticipation of a future pandemic during their careers.
Acknowledgments
Author Contributions: Author M.S. took the lead in writing the manuscript and performed the analyses. Authors M.S., K.F., C.M., and C.F. were key in shaping the research questions. All authors contributed and provided critical feedback to the manuscript. C.M. provided consultation on the analyses.
The authors thank Kathleen Silver for her outstanding assistance in preparing and submitting this manuscript.
References
- Lash RR, Donovan CV, Fleischauer AT, et al; Contact Tracing Assessment Team. COVID-19 contact tracing in two counties—north Carolina, June–July 2020. MMWR Morb Mortal Wkly Rep. 2020;69(38):1360-1363. doi:10.15585/mmwr.mm6938e3
- Staes CJ, Gesteland PH, Allison M, et al. Urgent care providers’ knowledge and attitude about public health reporting and pertussis control measures: implications for informatics. J Public Health Manag Pract. 2009;15(6):471-478. doi:10.1097/PHH.0b013e3181af0aab
- Schwenk TL. Public health—the role of family physicians. Am Fam Physician. 2003;68(10):1926, 1929-1930.
- Parton HB, Perlman SE, Koppaka R, Greene CM. Putting public health into practice: a model for assessing the relationship between local health departments and practicing physicians. Am J Public Health. 2012;102(S3)(suppl 3):S333-S335. doi:10.2105/AJPH.2011.300645
- Vickery KD, Rindfleisch K, Benson J, Furlong J, Martinez-Bianchi V, Richardson CR. Preparing the next generation of family physicians to improve population health. Fam Med. 2015;47(10):782-788.
- Accreditation Council for Graduate Medical Education. ACGME program requirements for graduate medical education in family medicine. Published 2020. Accessed August 12, 2021. https://acgme.org/Portals/0/PFAssets/ReviewandComment/RC/120_FamilyMedicine_2020-02-10_RC.pdf
- Macy ML, Huetteman P, Kan K. Changes in primary care visits in the 24 weeks after COVID-19 stay-at-home orders relative to the comparable time period in 2019 in metropolitan Chicago and Northern Illinois. J Prim Care Community Health. 2020;11:2150132720969557. doi:10.1177/2150132720969557
- Schad LA, Brady LA, Tumiel-Berhalter LM, et al. Impact of COVID-19 on Screening Rates for Colorectal, Breast, and Cervical Cancer: Practice Feedback From a Quality Improvement Project in Primary Care. J Patient Cent Res Rev. 2021;8(4):347-353. doi:10.17294/2330-0698.1856
- Frieden TR, Buissonnière M, McClelland A. The world must prepare now for the next pandemic. BMJ Glob Health. 2021;6(3):e005184. doi:10.1136/bmjgh-2021-005184
- Basu S, Phillips RS, Phillips R, Peterson LE, Landon BE. Primary care practice finances in yhe United States amid the COVID-19 Pandemic: study estimates the potential impact of COVID-19 on operating expenses and revenues of primary care practices. Health Aff (Millwood). 2020;39(9):1605-1614. doi:10.1377/hlthaff.2020.00794
- Seehusen DA, Mainous AG III, Chessman AW. Creating a centralized infrastructure to facilitate medical education research. Ann Fam Med. 2018;16(3):257-260. doi:10.1370/afm.2228
- Krist AH, DeVoe JE, Cheng A, Ehrlich T, Jones SM. Redesigning primary care to address the COVID-19 pandemic in the midst of the pandemic. Ann Fam Med. 2020;18(4):349-354. doi:10.1370/afm.2557
- Rawaf S, Allen LN, Stigler FL, Kringos D, Quezada Yamamoto H, van Weel C; Global Forum on Universal Health Coverage and Primary Health Care. Lessons on the COVID-19 pandemic, for and by primary care professionals worldwide. Eur J Gen Pract. 2020;26(1):129-133. doi:10.1080/13814788.2020.1820479
- Kretzschmar ME, Rozhnova G, Bootsma MCJ, van Boven M, van de Wijgert JHHM, Bonten MJM. Impact of delays on effectiveness of contact tracing strategies for COVID-19: a modelling study. Lancet Public Health. 2020;5(8):e452-e459. doi:10.1016/S2468-2667(20)30157-2
- Kozakowski SM, Eiff MP, Green LA, et al. Five key leadership actions needed to redesign family medicine residencies. J Grad Med Educ. 2015;7(2):187-191. doi:10.4300/JGME-D-14-00214.1
- Prunuske J, Chang L, Mishori R, Dobbie A, Morley CP. The extent and methods of public health instruction in family medicine clerkships. Fam Med. 2014;46(7):544-548.
- Nonpharmaceutical Interventions (NPIs). Centers for Disease Control and Prevention. Published April 27, 2020. Accessed January 26, 2022. https://www.cdc.gov/nonpharmaceutical-interventions/index.html
- Public health pathways for residents. Association of American Medical Colleges. Published 2021. Accessed July 6, 2021. https://students-residents.aamc.org/training-residency-fellowship/article/public-health-pathways-3
- Certificates of Added Qualification (CAQ). American Association of Family Physicians. Published 2021. Accessed July 6, 2021. https://www.aafp.org/about/policies/all/certificates-of-added-qualification.html
- Rankin WM, Cochrane A, Puffer JC, Puffer JC. Family physicians with a Certificate of Added Qualifications (CAQs) in sports medicine spend an increasing amount of their time practicing sports medicine. J Am Board Fam Med. 2015;28(6):695-696. doi:10.3122/jabfm.2015.06.150179
- Peterson LE, Cochrane A, Bazemore AW, Petterson S. Reported practice patterns among family physicians with a geriatrics certificate of added qualifications. J Am Board Fam Med. 2015;28(3):314-315. doi:10.3122/jabfm.2015.03.140333
- Morley CP, Rosas SR, Mishori R, et al. Essential public health competencies for medical students: establishing a consensus in family medicine. Teach Learn Med. 2017;29(3):255-267. doi:10.1080/10401334.2016.1268964
- Setia MS. Methodology series module 3: cross-sectional studies. Indian J Dermatol. 2016;61(3):261-264. doi:10.4103/0019-5154.182410




There are no comments for this article.