Background and Objectives: Distance learning is a feasible and effective method of delivering education, especially in rural settings. Few studies focus on remote learning in graduate medical education. This study explores remote didactic practices of rural family medicine programs in the United States.
Methods: We conducted an electronic survey of rural family medicine residency site directors across the United States. We completed sample analyses through descriptive statistics with an emphasis on descriptions of current didactic practices, facilitators, and challenges to implementation.
Results: The overall response rate was 38% (47/124) for all participants from rural residency programs, representing 28 states. About 24% of rural training track (RTT) participants reported no shared remote didactics between urban and rural sites. More than half of RTT participants (52%) reported remote virtual didactics were either not shared between urban and rural site or were shared less than 50% of the time. Top challenges to implementing remote shared didactics were lack of appropriate technology (31%) and lack of training for faculty and residents in delivery of remote didactics (31%). Top facilitators included having technology for the remote connection (54%), a faculty champion (42%), and designated time to develop the curriculum (38%).
Conclusions: There is potential for improving shared remote didactic sessions between rural and urban sites for family medicine RTTs, which may enhance efficiency of curriculum development across sites and maximize opportunities for bidirectional learning between urban and rural sites.
The United States is currently experiencing a primary care provider shortage, with projections of up to 55,000 too few primary care physicians by the year 2033.1 The provider shortage dramatically impacts rural communities, where access to medical providers is limited.2,3 To address the shortage of rural physicians, efforts are underway to increase recruitment to rural areas and expand rural medical and residency training.4-9 As the need and desire to create more rural programs grows, so does the need for feasible and effective didactic curricula that can provide rural residents with necessary training and education.
Rurally-focused family medicine residencies, such as rurally-located residency programs and rural training tracks (RTT), improve the pipeline and retention of rural practicing family physicians.5, 10-12 An RTT, also named “integrated rural training track” (IRTT), is a training program that includes training time at a large urban center with the majority of time spent at a rural site(s).12 Using the definition proposed by Longenecker,13 an RTT must be a separately-accredited residency program from the partnering urban site residency. Residents in an RTT spend at least 50% of their training time in a rural location, and programming in the rural sites must be “substantially integrated” with the urban site, which includes shared didactics and/or scholarly activity, a minimum of 4 months of shared curriculum, some sharing of a faculty or program director, and structured interaction of residents between the urban and rural sites.13 In rural areas, residency programs highly value quality teaching and training, but it can be difficult to recruit, retain, and support enough faculty to provide the necessary teaching as productivity demands and burnout have been reported as risk factors to RTT program closures.14 Sharing educational efforts and resources between faculty at urban and rural sites may help distribute and alleviate the responsibility placed on faculty, and could help ensure the quality and broad scope of resident training.
Distance learning, also commonly referred to as elearning, telelearning, and remote learning, occurs when instructors and learners are located in different places and interact using technology. Previous studies demonstrate the feasibility and effectiveness of a remote learning format; however, many of these studies focus on K-12, undergraduate programs, or international programs.15 Of those that highlight US medical training programs, most focused on individual online courses/electives, asynchronous models, or blended (asynchronous and synchronous) curricula.16-23 To the best of our knowledge, there are no recent studies examining how US rural family medicine residencies are using distance learning modalities to deliver didactics. This study seeks to illuminate the current didactics practices of rural family medicine residency programs across the country, with a specific focus on RTTs and remote didactics delivery, and to evaluate the facilitators and challenges to implementing and utilizing remote didactics.
We conducted five key informant telephonic interviews with program directors and residents from RTT programs to inform and guide the development of an electronic survey. Key informant interviews were conducted from August 2019 through September 2019 and lasted between 30 and 45 minutes each. Participants were recruited through convenience sampling with efforts to recruit participants representing US regional diversity. We used a semistructured interview guide for key informant interviews focusing on the experience and model for didactics delivery at urban and rural residency sites, technology used for shared didactics if didactics were shared between sites, and training for remote didactics delivery. We performed thematic analysis on the transcripts and notes from the interviews, and findings from the interviews informed electronic survey development.
We conducted a national cross-sectional survey of program directors and faculty from rural residency training programs using contact information from the RTT Collaborative.12 We used the list of programs maintained and published by the RTT Collaborative website24 because there is no Accreditation Council for Graduate Medical Examination-endorsed list of all current RTT programs available for public use. The survey was open from January 2020 through March 2020 and was sent to 124 working email addresses representing 107 unique training programs. Participants were asked to answer a series of questions regarding current shared and remote didactic practices and facilitators and challenges to implementing shared remote didactics across urban and rural sites; data were collected, stored, and managed via REDCap (Research Electronic Data Capture).25
We collected demographic data including participant age, years of postresidency practice, and program-specific characteristics, including urban site residency program type, distance between urban and rural training sites, and approximate size of rural community served by rural training sites. Outcomes of interest included various characteristics of shared didactics, including the proportion of remote didactics and in-person didactics, and the frequency, duration, and format of shared didactic sessions. We also asked about challenges and facilitators to implementing remote shared didactics.
After the survey closed, we excluded from our analysis submissions that were incomplete. For the survey question asking participants to choose their program type, we utilized the categories suggested by Longnecker7 for the answer choices (ie, rurally-located program, rural training pathway, RTT, rural-centric program, or other). However, in practice, there is an absence of shared nomenclature delineating the types of rural family medicine training programs, and this was evident in review of participants’ responses. In preliminary review of our data, we noticed discrepancies among participants’ self-reported program type and descriptive program characteristics used to help define the type of rural training program, such as length of time residents spend at a rural training site and the number of residents at the rural sites. With this in mind, we recategorized the program-type variable for some participants. Any participants reporting that their programs had some residents at rural sites during residency years 2 and 3 and reporting at least 18 months of training for each resident at rural sites were categorized as RTTs.13
We used descriptive statistics to evaluate sample characteristics, and Fisher’s Exact Test was used to compare the challenges and facilitators to implementing remote shared didactics among RTT programs by participants’ primary site of practice (rural vs urban), with significance level defined as P<.05. The University of Washington Human Subjects Division deemed this study exempt under category 2 of the Institutional Review Board exemption criteria.
We received a total of 52 responses from participants. Five surveys were incomplete and thus excluded, leaving 47 responses for analysis. Using these, the overall response rate was 38% (47/124) for all participants from rural residency programs representing 28 states with regional diversity across the United States, including the Northeast, Northwest, Midwest, Southeast, and Southwest. Of note, we received responses from 29 of 31 separately-accredited RTTs that existed as of January 2020. Responses from four RTT programs were received from both urban and rural site program directors(PDs)/associate program directors(APDs), creating duplicates in our data set. The decision was made to keep only the program directors’ responses for the analyses after comparing responses by both PD and APD and finding no significant differences. Thus, we included a total of 43 responses in the final analysis.
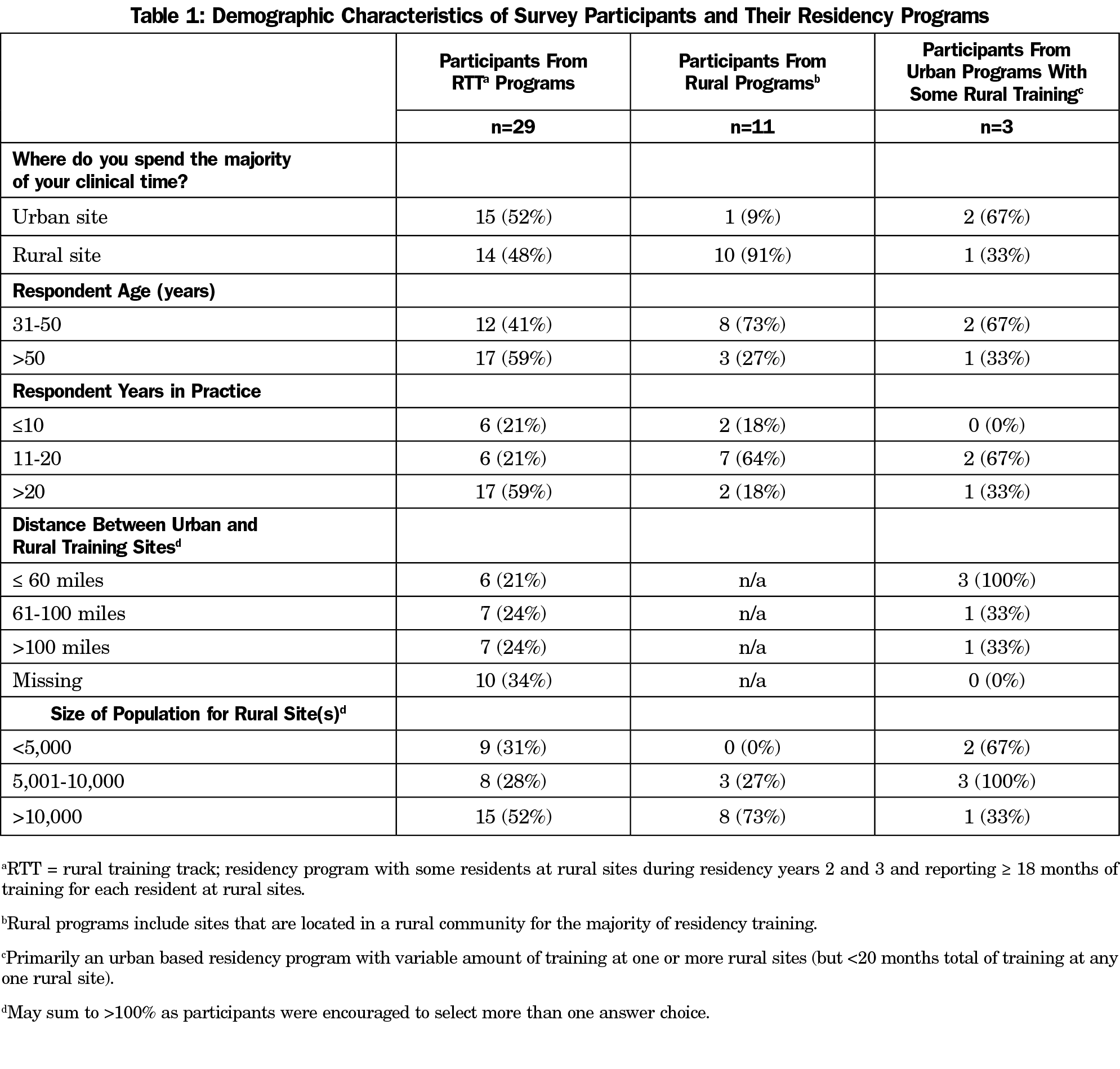
Table 1 shows the demographics of participants and self-reported program and practice-specific characteristics from all programs. Respondents from RTT programs represented 67% (29/43) of all participants, with approximately half (48%) of participants primarily practicing in rural settings and almost one-third (31%) practicing in highly-remote settings (ie, rural sites serving populations of less than 5,000 people). Participants self-identified as program directors (n=33, 77%), associate program directors (n=6, 14%), and other core faculty (n=4, 9%). Most participants from RTT programs were older than 50 years (59%) and had been practicing for more than 20 years (59%). About one-quarter (24%) of participants from RTT programs reported that the distance from rural to urban training sites was greater than 100 miles. Missingness was high for this question (n=10, 34%) because of the recategorization of program type as the survey was set to skip this question for participants who did not self-designate as a rural training track. About 52% of RTT participants and 73% of rural residency program participants reported the size of the population in their rural sites exceeded 10,000 people.
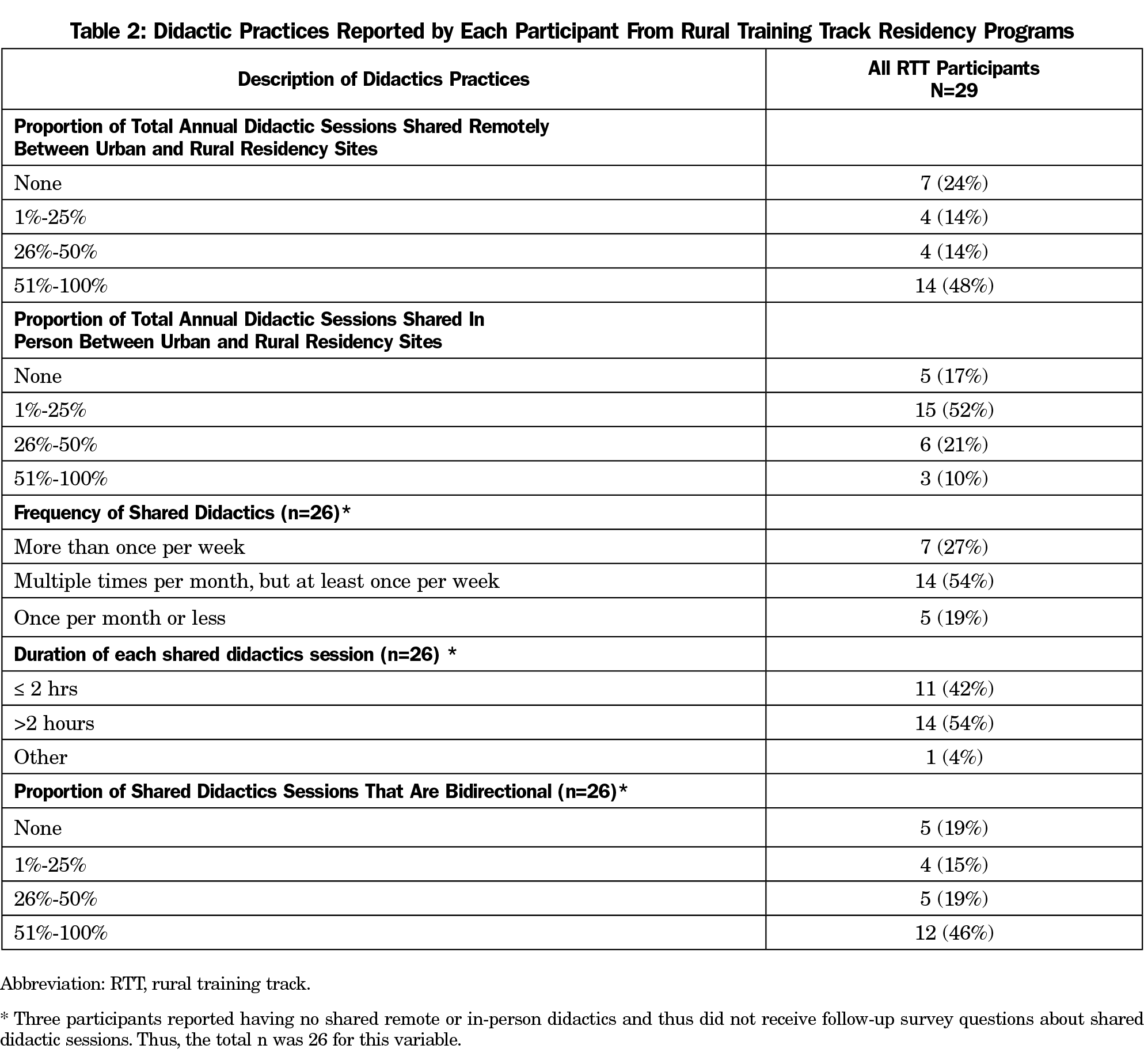
We chose to focus on RTT programs for the remainder of the analysis because of the small number of participants from the other types of programs and the difference in structure of the other programs (eg, variability in expectations of shared didactics, etc). A description of didactics practices at all RTT programs is shown in Table 2. All participants from RTT programs reported that their residency didactics are conducted synchronously (ie, in real-time). About one-quarter (24%) of participants reported having no shared remote didactics between urban and rural sites. The majority (81%) of RTT participants who reported having shared in-person, shared remote didactics, or both, held their shared didactics sessions more frequently than once per month. The majority (81%) of participants reported that some of their shared didactics (range of 1%-100%) were bidirectional in format. The didactic formats most commonly used at RTT programs included lecture-based didactics (n=26, 90%) and interactive discussions (n=21, 72%), while the least common format used was flipped classroom (n=2, 7%).
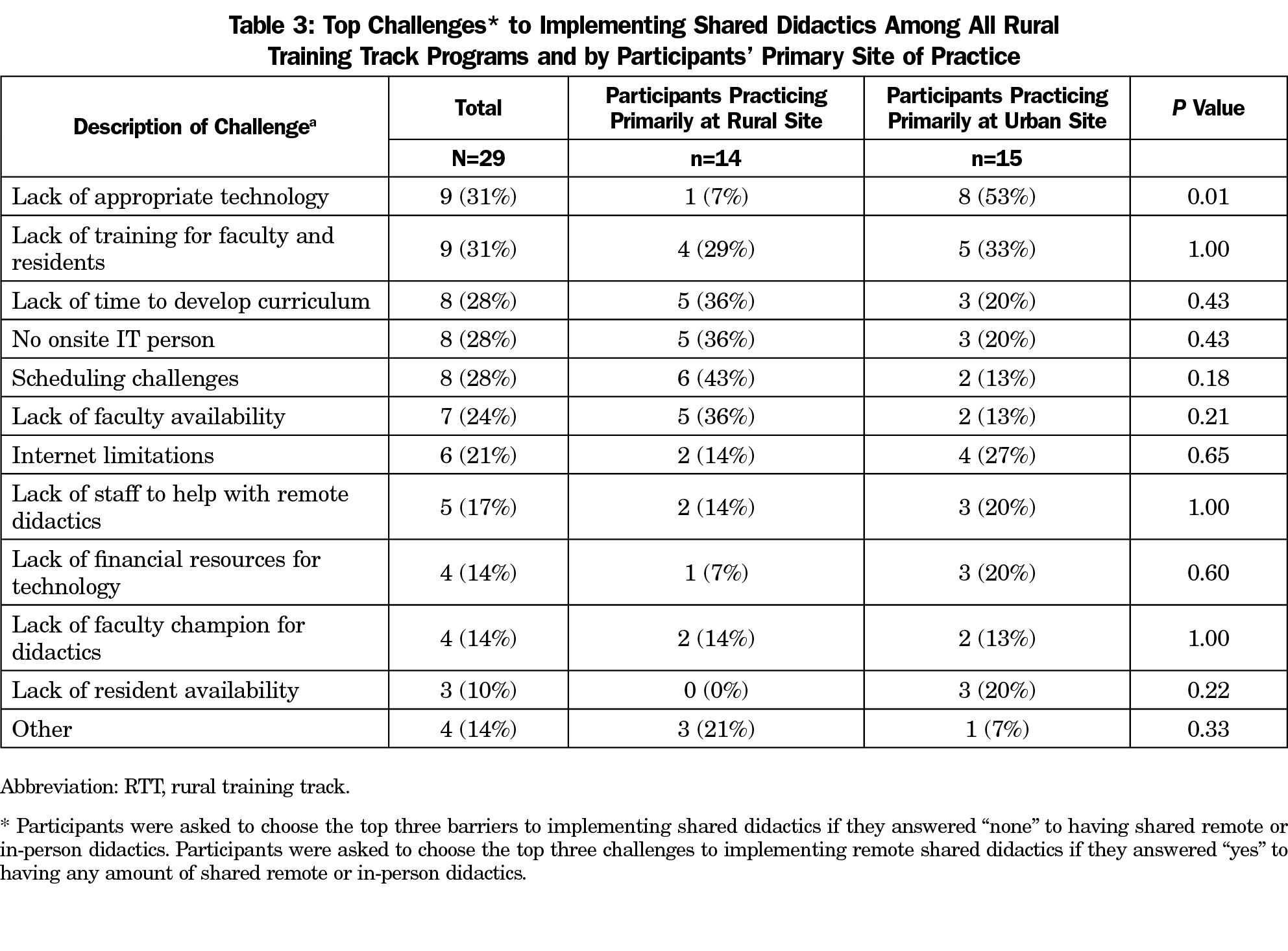
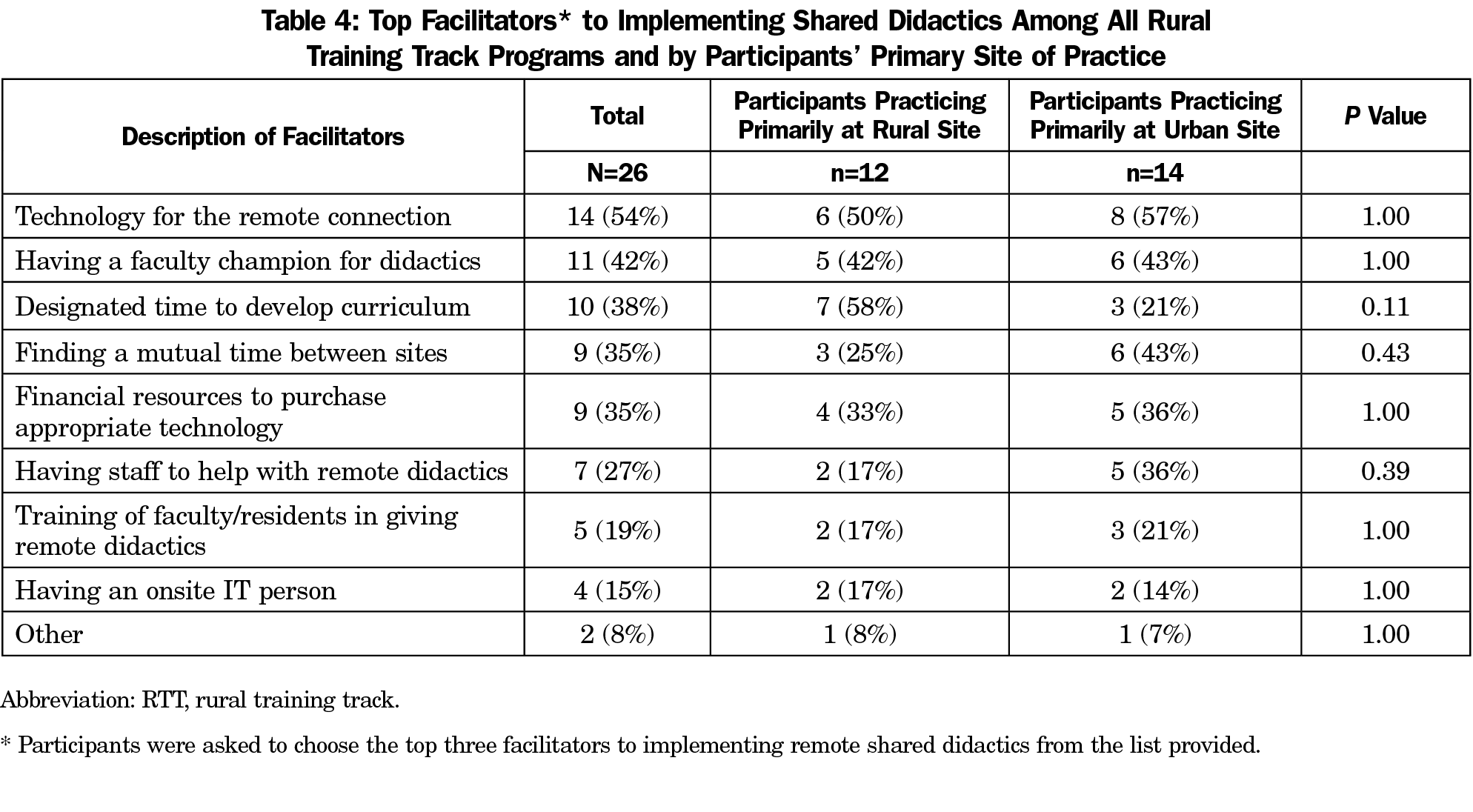
We explored challenges to implementing remote shared didactics for RTT programs (Table 3) and found the top challenges for all programs to be lack of appropriate technology (31%) and lack of training for faculty and residents in delivery of remote didactics (31%). However, the top challenges for participants practicing primarily in rural sites were different as compared with those practicing primarily in urban sites. Rural site participants chose “scheduling challenges” as the top barrier while urban site participants chose “lack of appropriate technology” as the top barrier. The only significant difference among the challenges reported by participants in rural and urban sites was the “lack of appropriate technology,” which was more frequently reported by participants primarily practicing in urban sites (P=.01). Among all RTT programs, the most frequently chosen facilitators to having shared remote didactics included having technology for the remote connection (54%), having a faculty champion (42%), and having designated time to develop the curriculum (38%). Rural site participants chose “designated time to develop the curriculum” most often, while urban site participants chose “having technology for the remote connection” most often as facilitators (Table 4). There were no significant differences in the choices of top facilitators between participants primarily practicing at the urban sites compared to participants primarily practicing at rural sites.
Additionally, we found that only 52% of RTT participants were satisfied or very satisfied with the structure of didactics at their rural training sites and 81% were interested or very interested in holding shared remote didactics between urban and rural sites (data not shown in tables).
With the majority of participants from RTT programs and almost half of them practicing in a rural setting, our results provide important insight into how didactics are perceived in both urban and rural programs with some shared curricula and integrated programming. Our results show that most didactic sessions are not being shared in person or virtually between RTT programs’ urban and rural sites, which suggests there is potential for implementing and improving the total amount of shared remote didactic sessions. In addition, rural programs are not utilizing asynchronous didactics much or at all.
Challenges to remote delivery of didactics differ between urban and rural sites, and include the lack of appropriate technology (urban) and finding time to coschedule didactics (rural). Understanding technological barriers and considering asynchronous didactic offerings21-23, 26 may be steps toward addressing these barriers and providing effective clinical education for family medicine residents and faculty.
Common facilitators to the success of shared remote didactics among all participants include the presence of a faculty champion and effective technology for transferring information over a remote connection. Designated time to develop curricula (rural) and ability to schedule a common time for didactics (urban) were other factors promoting successful shared remote didactics. Rural community physicians are responsible for a broad scope of practice and often must manage complex patient needs with limited access to specialty consults and advanced diagnostic studies27,28; consequently, RTT residents and faculty offer unique lessons on the of delivery of medical care in a resource-limited setting. Increased dialogue between rural and urban sites may offer important insights for residents, faculty, and the future of family medicine practice in both settings.
Results from this study are timely and important as the Health Services and Resources Administration is funding the expansion of rural primary care residency programs and family medicine RTTs through the Rural Residency Planning and Development (RRPD) program.29 Newly developed RTTs will need effective didactic curricula that provide rural residents with necessary training and education. Remote shared didactics between urban and rural sites may fulfill this need while encouraging faculty and resident cross-site collaboration and bidirectional learning. Given less than 20% of RTT graduates are engaged in teaching/medical education after graduation,30 future studies may evaluate how remote, bidirectional didactics could contribute to faculty retention and satisfaction with teaching. Ultimately, for programs exploring increased use of shared remote didactics, we suggest prioritizing the following factors that may improve successful implementation and utilization:
- Address underlying technological limitations, such as training for residents and faculty and designation of an IT staff member to help with the remote connection when needed;
- Attention to coordinated scheduling between sites; and
- Appointment of a faculty champion and provision of protected time to develop the curriculum.
Limitations of the study include self-reporting of program type, relatively small sample size, and timing of survey prior to the COVID-19 pandemic. As the pandemic has inevitably resulted in a restructuring of the delivery of didactics education across all graduate medical education to more remote learning platforms, it is highly likely that the findings of this survey would demonstrate higher levels of utilization of remote shared didactics at this time. However, the challenges and facilitators identified in this study and their implications likely remain unchanged.
This national survey study is the first to describe remote didactics practices among rural family medicine training programs. With less than half of participants from rural family medicine training programs utilizing shared remote didactics and a bidirectional didactics format, there may be room for improvement in sharing of resources (eg, faculty and resident teaching time) and improving efficiency for didactics delivery. Future studies may focus on evaluating the influence of differential resource allocation and availability based on location or university affiliation of RTT programs and other rural family medicine residency programs, exploring remote didactic best practices and the criteria for determining excellence in remote didactics delivery, and investigating the rapid changes brought on by the COVID-19 pandemic in virtual learning.
Acknowledgments
This research was supported by the Bureau of Health Workforce (BHW), Health Resources and Services Administration (HRSA), US Department of Health and Human Services (HHS) under cooperative agreement #UH1HP29966. The information, conclusions, and opinions expressed in this presentation are those of the authors and no endorsement by BHW, HRSA, or HHS is intended or should be inferred. We also acknowledge grant support (UL1 TR002319, KL2 TR002317, and TL1 TR002318 from the National Center for Advancing Translational Sciences/National Institutes of Health) for the electronic platform REDCap, which we used for survey data collection and storage for this study.
Financial Support: This research was supported by the BHW, HRSA, HHS under cooperative agreement #UH1HP29966.
Presentations: This study was presented as follows: Evaluation of Current Practices for Distance Learning Didactics Curricula in Rural Family Medicine Residency Programs, Annual RTT Collaborative National Conference, Virtual Meeting, April 16, 2020. “Best Practices for Implementing a Bidirectional Distance Learning Didactics Curriculum in Family Medicine Residencies”, STFM Annual Spring Conference (virtual), May 2021.
References
- Association of American Colleges. The Complexities of Physician Supply and Demand: Projections From 2018 to 2033. 2020. Accessed December 20, 2020. https://www.aamc.org/data-reports/workforce/data/complexities-physician-supply-and-demand-projections-2018-2033
- Petterson SM, Phillips RL Jr, Bazemore AW, Koinis GT. Unequal distribution of the U.S. primary care workforce. Am Fam Physician. 2013;87(11).
- Skinner L, Staiger DO, Auerbach DI, Buerhaus PI. Implications of an aging rural physician workforce. N Engl J Med. 2019;381(4):299-301. doi:10.1056/NEJMp1900808
- Longenecker RL, Schmitz D. Building a community of practice in rural medical education: growing our own together. Rural Remote Health. 2017;17(1):4195. doi:10.22605/RRH4195
- Hawes EM, Fraher E, Crane S, et al. Rural Residency Training as a Strategy to Address Rural Health Disparities: Barriers to Expansion and Possible Solutions. J Grad Med Educ. 2021;13(4):461-465. doi:10.4300/JGME-D-21-00274.1
- Meyers P, Wilkinson E, Petterson S, et al. Rural workforce years: quantifying the rural workforce contribution of family medicine residency graduates. J Grad Med Educ. 2020;12(6):717-726. doi:10.4300/JGME-D-20-00122.1
- Longenecker RL, Andrilla CHA, Jopson AD, et al. Pipelines to pathways: medical school commitment to producing a rural workforce. J Rural Health. 2021;37(4):723-733. doi:10.1111/jrh.12542
- Hawes EM, Weidner A, Page C, et al. A roadmap to rural residency program development. J Grad Med Educ. 2020;12(4):384-387. doi:10.4300/JGME-D-19-00932.1
- Health Resources and Services Administration. Rural Residency Planning and Development (RRPD) Program Awards. Accessed December 8, 2021. https://www.hrsa.gov/rural-health/research/rrpd-awards
- Patterson DG, Schmitz D, Longenecker R, Andrilla CHA. Family medicine rural training track residencies: 2008-2015 graduate outcomes. Seattle, WA: WWAMI Rural Health Research Center, University of Washington; February 2016.
- Parlier AB, Galvin SL, Thach S, Kruidenier D, Fagan EB. The road to rural primary care: a narrative review of factors that help develop, recruit, and retain rural primary care physicians. Acad Med. 2018;93(1):130-140. doi:10.1097/ACM.0000000000001839
- The RTT Collaborative. What is a Rural Program? Accessed June 10, 2019. https://rttcollaborative.net/rural-programs/#participating-programs
- Longenecker R. Rural medical education programs: a proposed nomenclature. J Grad Med Educ. 2017;9(3):283-286. doi:10.4300/JGME-D-16-00550.1
- Patterson DG, Schmitz D, Longenecker RL. Family medicine rural training track residencies: risks and resilience. Fam Med. 2019;51(8):649-656. doi:10.22454/FamMed.2019.769343
- Nguyen T. The effectiveness of online learning: Beyond no significant difference and future horizons. MERLOT Journal of Online Learning and Teaching. 2015;11(2)-309-319.
- Kunin M, Julliard KN, Rodriguez TE. Comparing face-to-face, synchronous, and asynchronous learning: postgraduate dental resident preferences. J Dent Educ. 2014;78(6):856-866. doi:10.1002/j.0022-0337.2014.78.6.tb05739.x
- Klein KP, Hannum WM, Koroluk LD, Proffit WR. Interactive distance learning for orthodontic residents: utilization and acceptability. Am J Orthod Dentofacial Orthop. 2012;141(3):378-385. doi:10.1016/j.ajodo.2011.08.028
- Markova T, Roth LM, Monsur J. Synchronous distance learning as an effective and feasible method for delivering residency didactics. Fam Med. 2005;37(8):570-575.
- Motycka CA, St Onge EL, Williams J. Asynchronous versus synchronous learning in pharmacy education. Journal of Curriculum and Teaching. 2013;2(1):63-67. doi:10.5430/jct.v2n1p63
- Wray A, Bennett K, Boysen-Osborn M, Wiechmann W, Toohey S. Efficacy of an asynchronous electronic curriculum in emergency medicine education in the United States. J Educ Eval Health Prof. 2017;14:29. doi:10.3352/jeehp.2017.14.29
- Chang TP, Pham PK, Sobolewski B, et al. Pediatric emergency medicine asynchronous e-learning: a multicenter randomized controlled Solomon four-group study. Acad Emerg Med. 2014;21(8):912-919. doi:10.1111/acem.12434
- Lebensohn P, Kligler B, Brooks AJ, et al. Integrative medicine in residency: feasibility and effectiveness of an online program. Fam Med. 2017;49(7):514-521.
- Dawson A, Mullen K, Janson IA, et al. A feasibility pilot study of online modules of hydroxyurea and sickle cell disease care for adolescents and young adults for family medicine residents. J Pediatr Hematol Oncol. 2021.
- The RTT Collaborative. Listing of Participating Programs. Updated July 2020. Accessed April 30, 2021. https://rttcollaborative.net/rural-programs/
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. doi:10.1016/j.jbi.2008.08.010
- Chiasson AM, Brooks AJ, Ricker M, Lebensohn P, Chen MK, Maizes V. Educating physicians in family medicine residencies about nonpharmacologic approaches to pain: results of an online integrative course. Fam Med. 2020;52(3):189-197. doi:10.22454/FamMed.2020.865003
- Wendling AL. Rural matters. Fam Med. 2016;48(8):593-595.
- Iglehart JK. The Challenging quest to improve rural health care. N Engl J Med. 2018;378(5):473-479. doi:10.1056/NEJMhpr1707176
- Johnson S, Pauwels J, Nolan D. Bridging the physician workforce in rural America. Federal Office of Rural Health Policy Grant; 2021.
- Patterson DG, Longenecker R, Schmitz D, et al. Policy brief: Rural residency training for family medicine physicians: graduate early-career outcomes. Seattle, WA: WWAMI Rural Health Research Center, University of Washington. Jan 2012 (revised). http://depts.washington.edu/uwrhrc/uploads/RTT_Grad_Outcomes_PB.pdf



There are no comments for this article.