Background and Objectives: Empathy is considered a prerequisite for a successful physician-patient relationship. The Jefferson Scale of Patient Perceptions of Physician Empathy (JSPPPE) is a regularly-used, patient-rated measure of physician empathy. The aim of this study is to translate and analyze the reliability and validity of the JSPPPE Spanish (Spain) version (Sp-JSPPPE) in primary care in order to use it with medical trainees.
Methods: After translation and back translation of the JSPPPE, 369 patients from 21 primary care physicians in Pamplona (Navarre, Spain) completed the Sp-JSPPPE, a sociodemographic questionnaire, the Spanish (Spain) Consultation and Relational Empathy Measure (Sp-CARE), and a question about overall satisfaction. We studied internal reliability (Cronbach’s α and ordinal α), homogeneity (corrected item-total correlations), construct validity (confirmatory factor analysis [CFA]) and concurrent validity (Spearman’s correlation) of Sp-JSPPPE.
Results: Cronbach’s α and ordinal α were 0.870 and 0.919, respectively, for the Sp-JSPPPE, and all corrected item-total correlations exceeded the accepted cutoff of 0.30, demonstrating high internal reliability and homogeneity. CFA corroborated the one-factor structure proposed in the original version. The total score for the Sp-JSPPPE was significantly correlated with sp-CARE (Spearman’s ϱ 0.651, P<.001) and with overall patient satisfaction (Spearman’s ϱ 0.504, P<.001).
Conclusions: The results support the reliability and validity of the Sp-JSPPPE in primary care. Sp-JSPPPE could be useful in empathy assessment of medical trainees, both graduate and postgraduate, in the Spanish context.
A successful doctor-patient relationship requires physicians to maintain good interpersonal and communication rapport.1 Patients appreciate their physician’s dedication, which includes listening, explaining clearly, and involving patients in decision making.2
Empathy is considered a prerequisite for a successful physician-patient relationship.3,4 It is the most frequently mentioned personal quality when describing a “humanistic physician,” and is a major element of professionalism in medicine.5
Empathy is not clearly or universally defined, but some of its key components are unanimously recognized. In the context of patient care, it involves striving to understand patients’ “experiences, concerns, and perspectives, combined with the capacity to communicate this understanding, and an intention to help.”6
Empathy has been associated with improved patient satisfaction,7–9 increased adherence to treatment,10–12 and improved clinical outcomes.13–15 It has also been associated with decreased litigation16 and less acute clinical burnout among physicians,17,18 thereby benefitting clinicians’ well-being.12,17,19
Physician empathy may be assessed either through self-reported, patient-reported, or observer-reported measures. The correlation between these three different kinds of measures varies.7,20 Patient viewpoints are essential to contemplate patient expectations, which can be key in attaining successful clinical results. It should also be noted that physician self-assessments of empathy do not always correlate exactly with patient-reported assessments.20 A great number of factors often influence the patient perspective apart from direct physician interaction, such as, overall physical environment, gender (the patient’s or physician’s), and the length and context of the consultation.21
The Jefferson Scale of Patient Perceptions of Physician Empathy (JSPPPE), which was developed as a brief instrument (5-items) that patients can complete in a few minutes after clinical consultation,22 is now available in several languages,23 including Spanish (Argentina).24 However, it has not been translated and validated in Spanish (Spain) and language differences between countries are important. There are some expressions, ways of talking, and individual words, that may change the meaning of the items.25,26 A proper translation is important as suggested by other authors for JSE-s scale.27 Other studies showed differences in the self-assessment of empathy between Spain and other Latin American countries. Some factors involved in the development of empathy are sensitive to cultural influence. In the area of health, the complex economic, political, social and cultural framework of Latin America poses a constant challenge and may favor empathy to be lower.28,29 However, the main reason for translation and validation is language differences.
This article aims to report the translation of the JSPPPE into Spanish (Spain) and the study of the scale’s reliability and validity. We conducted this translation and validation with the inestimable help of family medicine tutors and primary care settings directors, who wanted to have a validated tool to improve family physicians’ empathy in the Spanish context.
Translation of the JSPPPE
The JSPPPE22,30 consists of five items:
- Can view things from my perspective (see things as I see them);
- Asks about what is happening in my daily life;
- Seems concerned about me and my family;
- Understands my emotions, feelings and concerns; and
- Is an understanding doctor. Scored on a Likert scale from 1 (strongly disagree) to 7 (strongly agree).
The total score corresponds to the sum of each individual question’s score; higher scores indicate greater patient ratings of empathy of a physician.
The first step consisted in getting authorization for translation from the author of the original JSPPPE. This process then involved two forward translations carried out by independent translators, a subsequent reconciliation of the forward translations, and finally a back translation by a bilingual translator who had no knowledge of the measure’s original version. This last translation unveiled the inaccuracies present in the forward-reconciled translation via comparison of the back translation with the original version. The three translators then proceeded to discuss any discrepancies to attain a more refined version. This refined version was finally reviewed by two external, native Spanish speaker (Spain) experts. The final version was then pilot tested in a sample of 10 volunteer patients from one primary care center. These volunteers also completed an additional form related to the clarity of each item, whether they had found irrelevant or offensive material, or if they would like to suggest possible additional questions. Their feedback did not contain any significant suggestions or remarks so the final version remained unchanged.
Study Design and Participants
In the course of 4 months, we enlisted 21 volunteer primary care physicians (PCPs), who were specialists in family medicine and native Spanish (Spain) speakers. They worked in five primary care centers (within the public health system) in the city of Pamplona and its surrounding areas (Navarre, Spain).
A suitable sample of 369 patients was subsequently recruited through these PCPs; 292 were born in Navarre and 77 were born elsewhere in Spain. The inclusion criteria for patients required being a native Spanish (Spain) speaker between 18 and 75 years old, and having visited that physician on at least one occasion in the previous year.
Immediately after the consultation, patients who agreed to fill out the questionnaire about their PCP were lead into a private room where one researcher described the study, collected their informed consent, and administered a sociodemographic questionnaire (Table 1). Patients then filled out the Spanish (Spain) JSPPPE (Sp-JSPPPE) and the Spanish (Spain) CARE Measure (Sp-CARE), another patient-reported questionnaire recently translated and validated by our group.31 They were also asked about their overall satisfaction with the medical consultation using a 5-point Likert-type scale and about their perception of the consultation’s length (minutes).
This study observed the principles of the Declaration of Helsinki, previously obtaining ethical approval from the competent organism, the Navarre government’s Clinical Research Ethics Committee. (BPC, CPMP/ICH/135/95). All participants, both patients and physicians, signed an informed consent document beforehand. Before filling out the questionnaire, patients were given written and oral information regarding the questionnaire’s anonymity, as well as the research team’s promise to not share their answers with any of the physicians.
Statistical Analysis
We completed the statistical analysis of the results using IBM SPSS Statistics (v 22) software and the Stata 12.1 (ordalpha) statistical package. We set a at the value of 0.05 for every analysis.
To ensure the reliability and validity of a questionnaire, the most important and essential thing is construct validity.32 If the validation has already been done in the original language, a factor analysis is not necessary but a confirmatory analysis,33 as we do in this article.
Internal reliability measures how much items in a questionnaire are correlated, and as such, are measuring the same concept.33 We used the Stata 12.1 program (ordalpha) with code by Coveney,34 modified by one of the authors to compute the ordinal a coefficient of the Sp-JSPPPE’s reliability, as this coefficient is better suited for Likert-type scales35 and when there is a ceiling effect. Furthermore, to compare with other studies, Cronbach’s α values and removal of any of the 5 items to see if it weakened those values were used. Cronbach’s α >0.70 indicates good internal consistency.33 We also took a closer look at homogeneity with corrected item-total correlations in order to single out any items that did not agree with other items in the questionnaire. Values above 0.30 predict high correlation.36
Before proceeding with factor analysis, we used Kaiser–Meyer–Olkin (KMO) measures to evaluate the percentage of variance that arises from the underlying factors (KMO values of 0.6 and above are required).37
We evaluated construct validity, taking into account previous studies, by means of confirmatory factor analysis (CFA).24,38,39 We performed CFA with Stata 12.1. using structural equation modeling (SEM) on a polychoric correlation matrix, as well as with the estimation method considered to provide maximum likelihood thanks to its adequacy for ordinal data.40 For the evaluation of model data fit, we used model χ2 goodness of fit and approximate fit indices. Nonsignificant results from a χ2 test (P>.05) indicates great model fit, but it should be noted that χ2 values are very susceptible to fluctuation based on sample size. For this reason, χ2 was calculated with a degrees of freedom (df) ratio, χ2/df, where values indicate good model fit if they are <3.41 Additional approximate fit indices employed included the Tucker-Lewis index (TLI), as well as the comparative fit index (CFI), which is used to measure incremental fit (values above 0.95 are indicative of a good fit). We also used the root-mean-square error of approximation (RMSEA), which was selected to measure parsimonious fit (values equal to or below 0.06 imply a good fit).42
We assessed concurrent validity by correlating Sp-JSPPPE scores with Sp-CARE Measure scores and overall patient satisfaction (Spearman’s ρ). Values >0.7 assume a strong correlation, those between 0.30 and 0.70 a moderate one, and those <0.30 indicate a poor correlation.43
We conducted multivariable regression analyses on the Sp-JSPPPE scores to detect any interaction between patients’ demographic factors, physicians’ characteristics, and consultation length.
Patient Characteristics
We recruited 369 patients, 367 of whom completed the study. The average age was 52.69 years (SD=14.55; range: 18 to 75); 217 (59.1 %) were female and 150 (40.9 %) were male (Table 1).
Physician Characteristics
We recruited 21 PCPs, seven male and 14 female, who were on average 52.28 years old (SD=6.74; range: 32 to 63). They had an average of 22.91 years (SD=8.93) of active work experience in the primary care setting.
Consultation Characteristics
The mean Sp-CARE Measure score was 42.21 (SD=7.38; n=365). The overall satisfaction mean was 4.77 (SD=0.50) on a 5-point Likert-type scale. The mean self-reported consultation length was 11.58 minutes (SD=5.36; range: 3 to 30).
Spanish (Spain) JSPPPE
The Sp-JSPPPE is available in Appenix 1 (https://journals.stfm.org/media/5035/appendix-1-diez.pdf).
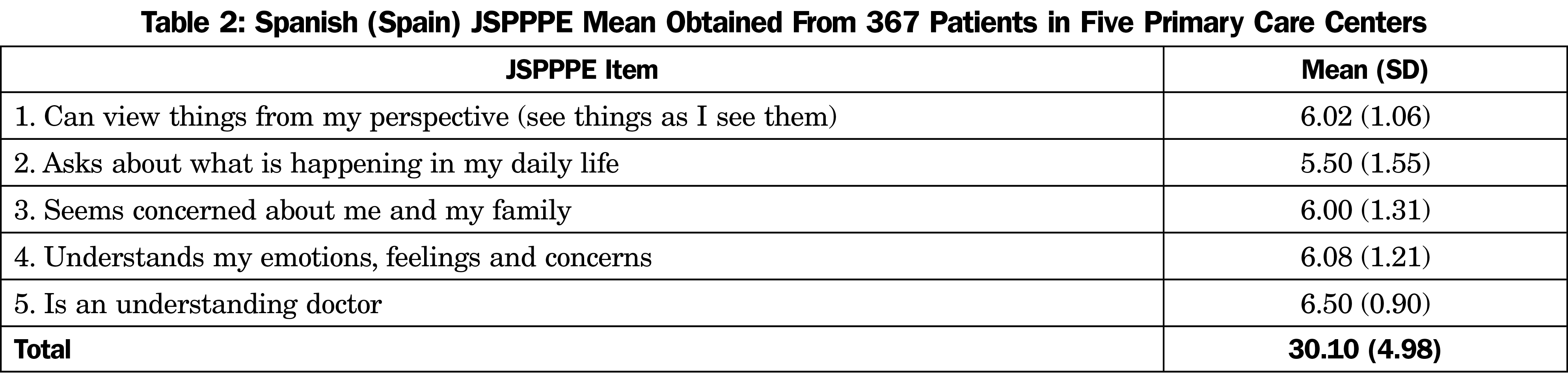
The mean Sp-JSPPPE score was 30.10 (SD=4.98) with an overall range from 9 to 35. Among all the items, the highest scores were found in item 5, “Is an understanding doctor,” mean 6.50 (SD=0.90), and the lowest scores were found in item 2 “Asks about what is happening in my daily life,” mean 5.50 (SD=1.55, Table 2). “Strongly agree” was the most common value (average of 49.4%).
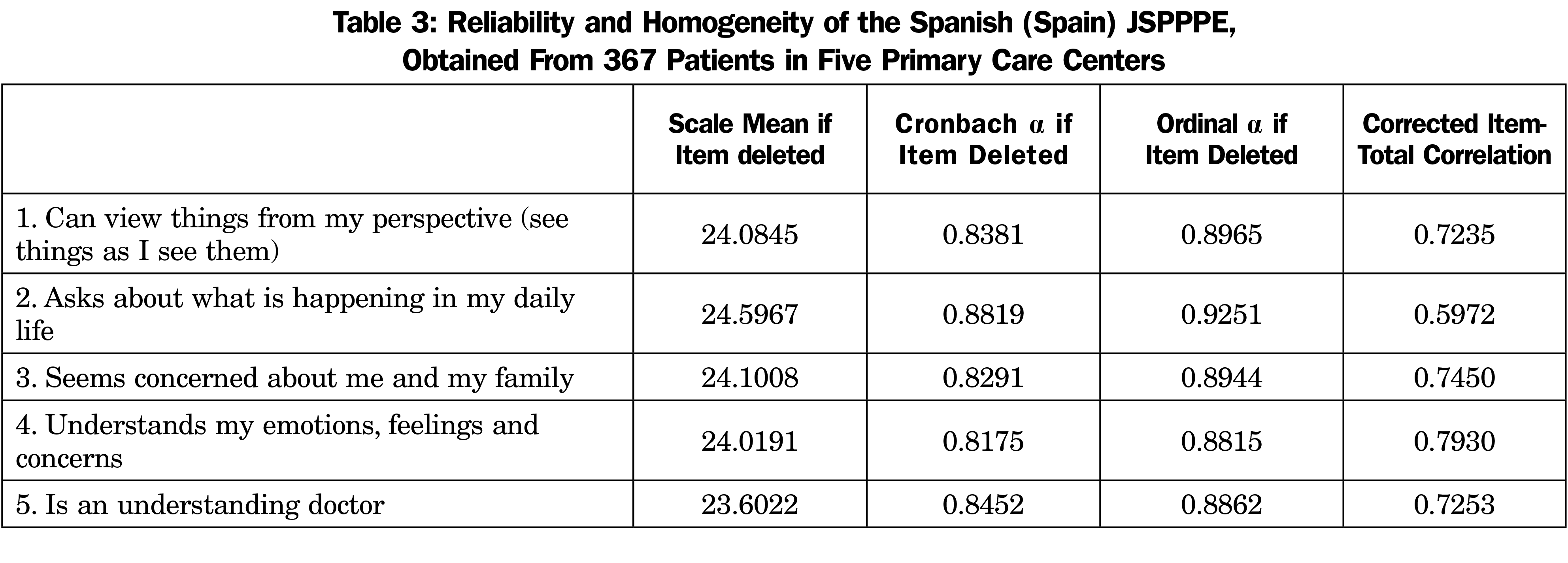
The internal reliability analysis for the 5 items on the Sp-JSPPPE, in terms of Cronbach’s α and ordinal α, were 0.870 and 0.919, respectively. Those values were moderately lowered with the deletion of any item, demonstrating high internal reliability. Ordinal α coefficients were slightly higher than Cronbach a. Every corrected item-total correlation exceeded 0.30—the acceptable cutoff point—indicating that all items appropriately contribute to the overall scale (Table 3).
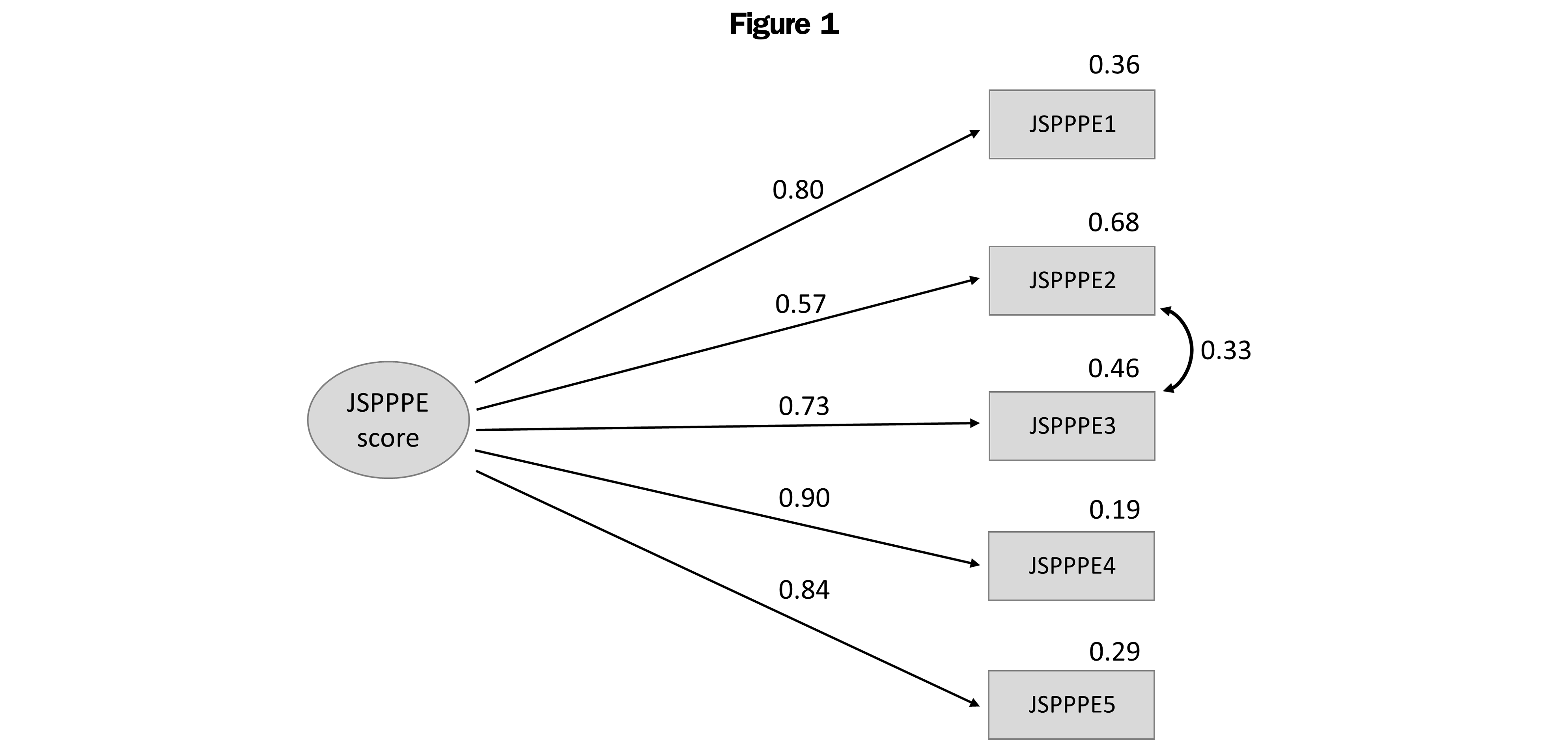
The KMO=0.851 result confirmed the adequacy of the data set for factor analysis. CFA indicated that the improved one-factor model (which admits some correlation between items’ errors) met the criteria, thus exhibiting a good fit: χ2(4)=10.28 (P=.034); χ2/df=2.57; CFI=0.994; TLI=0.985; RMSEA=0.065 (P<.05). Figure 1 demonstrates model fit.
In support of concurrent validity, the Sp-JSPPPE total score was significantly correlated with the Sp-CARE Measure (Spearman’s ρ 0.651, P<.001) and with overall patient satisfaction (Spearman’s ρ 0.504, P<.001).
Multivariable regression analysis (Table 4) revealed a significant relationship between Sp-JSPPPE scores and patients’ gender in that women perceived their physicians as more empathic than men (P=.006). Regarding physicians, those with more years of active practice were scored higher (P=.019). There were no differences based on the self-reported consultation length.
For this study, we translated the original version of the JSPPPE from English into Spanish (Spain) and analyzed its reliability and validity in primary care. This measure revealed high internal reliability, as well as construct validity.
One other study translated to Spanish (Argentina) and validated the measure using one 5-item version and one modified 6-item version of the instrument, both with a 5-point Likert-type answer scale.24 In addition to this difference in the Likert scale, language differences between countries are important. There are some expressions, ways of talking, and words that may change the meaning of the items, and is important an appropriate translation.
We resorted to the two most popular translation methods and cautiously merged them in order to translate the original JSPPPE from English into Spanish—this involved both one back translation and reconciliation of two forward translations. By this method, we obtained a translated version that respects every nuance in the original JSPPPE. Our pilot study, with a sample of 10 volunteers in a primary care setting in the city of Pamplona, corroborated the clarity and suitability of the Sp-JSPPPE for successful cultural adaptation.
The mean Sp-JSPPPE score was similar to the original scale’s results30,44,45 and to the mean obtained with other translations.38 Nevertheless, other versions have reported lower scores.46,47 Other empathy scales (CARE) also had lower values in Asian countries.48–50 Therefore, it seems that American and European countries obtain higher empathy patient-reported means than Asian countries.
Among the responses, “strongly agree” was the most common, demonstrating the presence of a ceiling effect. Therefore, we used an ordinal α coefficient, which is recommended when a ceiling effect is present. The original 5-point Likert scale questionnaires22 had a greater ceiling effect. Other studies also had a high ceiling effect,39 while articles that make no reference to this effect presented high mean scores.30,38 These results can be explained by the fact that Spanish (Spain) patients usually hold a positive view of their PCPs’ work. In fact, the community of Navarre, where the Sp-JSPPPE Measure was validated, attained the second highest score in a study involving satisfaction with the Spanish health care system.51
The highest scores were recorded for item 5, “Is an understanding doctor,” and the lowest score for item 2, “Asks about what is happening in my daily life,” results that mirror other studies.24,46,47 This may indicate that, although patients believed their physicians are understanding persons, they do not have enough time to ask about the problems influencing their health.
The internal reliability of the Sp-JSPPPE was established with a high Cronbach α (0.870) and ordinal α (0.919), and by the fact that removing any item results in a weaker alpha value. Corrected item total correlations were similarly high for all items (values above 0.30). We found similar results in the English version of the JSPPPE with a 7-point Likert scale,30,44,52,53 and with other languages.24,38,39,46,54
There was a clear hypothesis regarding the factor structure of the JSPPPE22 and we therefore performed CFA as indicated in literature.33 We found that the model has an appropriate fit, corroborating the one-factor structure proposed by the original version’s authors.22,30 We identified articles that involve JSPPPE translation and CFA validation24,38,39 with similar results.
We observed moderate correlation (r=0.651, P<.001) of JSPPPE scores in a primary health care setting with another empathy questionnaire, the Sp-CARE Measure, which has been widely used during general practice consultations. Studies looking at other medical specialties also found a correlation between both questionnaires.38,53 This correlation was expected and indicates that the two scales capture a related construct, contributing to the validity of the Sp-JSPPPE.
Concurrent validity manifested positive correlations in terms of patients’ overall satisfaction with their consultation (r=0.504). We assessed this with one question about overall satisfaction, (1-5) Likert-type scale, similar to another study.45 Keulen et al53 compared one question about overall satisfaction (0-10) and Hojat et al30 with an overall satisfaction scale (10 items) in the primary care setting. Other studies did so with the question, “Would you recommend the doctor to your family or friends?”24,30,46,47 finding good correlation among all of them. These findings are in line with the literature.5,9
Concerning patient characteristics, we only observed significant differences between the total Sp-JSPPPE score and patient gender. Similar to other study, female patients assigned higher JSPPPE scores than male patients.55 However, there are also studies in which males gave higher scores than females24,44 and some that found no differences.30,38,47,54 Clarifying such heterogeneous results between studies will require further studies with qualitative methodologies.
We found no association between the Sp-JSPPPE score and physicians’ characteristics. There is another study that evaluated it and found higher score in female physicians.38
Regarding physicians’ period of active practice, we found higher scores for physicians who were more experienced. We did not find other studies that measure this aspect. It is possible that more experienced physicians also had longer relationships with the patients. Unfortunately, this study did not collect such data.
Our study, like others,47,55 did not find any association between the Sp-JSPPPE score and patients’ perceptions of consultation length.
Strengths and Limitations
One central strength of this study corresponds to the amount of time and resources poured into coming up with a Spanish (Spain) translation of the English JSPPPE that is both precise and culturally meaningful. In fact, this involved a far more meticulous and thorough process than a simple translation and back translation. Another strength resides in having executed CFA to analyze construct validity in order to see if our Sp-JSPPPE truly adapts to the English version. We consequently discovered that both measures are indeed compatible. Moreover, the questionnaires were handed out by researchers and not by the physicians themselves, a methodological alternative that seeks to avoid the pressure that patients may otherwise feel, and which contributes to the questionnaires being successfully completed.
One limitation of the study is tied to the nature of the sample, a nonrepresentative population recruited from urban areas in one particular geographic location. Another limitation has to do with how the length of consultation was estimated (ie, by way of patients’ perceptions instead of more objective measures). Lastly, the number of times patients had visited their PCP in the previous year or the length of the relation between each patient and her/his doctor, were not considered in the study.
Our results support the reliability and validity of the Sp-JSPPPE as a patient-rated measure of empathy in the primary care setting. This validation study represents a first step in making the JSPPPE available to Spanish (Spain) speakers and can be considered in assessments of empathy in medical trainees, both graduate and postgraduate, in the Spanish context.
Acknowledgments
The authors are grateful to the PCPs, their staff, and their patients for participating in the study.
References
- Rathert C, Wyrwich MD, Boren SA. Patient-centered care and outcomes: a systematic review of the literature. Med Care Res Rev. 2013;70(4):351-379. doi:10.1177/1077558712465774
- Nowak DA, Sheikhan NY, Naidu SC, Kuluski K, Upshur REG. Why does continuity of care with family doctors matter? Review and qualitative synthesis of patient and physician perspectives. Can Fam Physician. 2021;67(9):679-688. doi:10.46747/cfp.6709679
- Wang Y, Wu Q, Wang Y, Wang P. The effects of physicians’ communication and empathy ability on physician-patient relationship from physicians’ and patients’ perspectives. J Clin Psychol Med Settings. 2022. doi:10.1007/s10880-022-09844-1
- Wu Q, Jin Z, Wang P. The relationship between the physician-patient relationship, physician empathy, and patient trust. J Gen Intern Med. 2021. doi:10.1007/s11606-021-07008-9
- Derksen F, Bensing J, Lagro-Janssen A. Effectiveness of empathy in general practice: a systematic review. Br J Gen Pract. 2013;63(606):e76-e84. doi:10.3399/bjgp13X660814
- Hojat M. Empathy in health professions education and patient care. Springer International Publishing; 2016, doi:10.1007/978-3-319-27625-0.
- Glaser KM, Markham FW, Adler HM, McManus PR, Hojat M. Relationships between scores on the Jefferson Scale of physician empathy, patient perceptions of physician empathy, and humanistic approaches to patient care: a validity study. Med Sci Monit. 2007 Jul;13(7):CR291-4.
- Hojat M, Louis DZ, Maxwell K, Markham FW, Wender RC, Gonnella JS. A brief instrument to measure patients’ overall satisfaction with primary care physicians. Fam Med. 2011;43(6):412-417. http://www.ncbi.nlm.nih.gov/pubmed/21656396
- Pollak KI, Alexander SC, Tulsky JA, et al. Physician empathy and listening: associations with patient satisfaction and autonomy. J Am Board Fam Med. 2011;24(6):665-672. doi:10.3122/jabfm.2011.06.110025
- Zolnierek KB, Dimatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009 Aug;47(8):826-34. doi: 10.1097/MLR.0b013e31819a5acc
- Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86(3):359-364. doi:10.1097/ACM.0b013e3182086fe1
- Gleichgerrcht E, Decety J. The relationship between different facets of empathy, pain perception and compassion fatigue among physicians. Front Behav Neurosci. 2014;8:243. doi:10.3389/fnbeh.2014.00243
- Hegazi I, Wilson I. Maintaining empathy in medical school: it is possible. Med Teach. 2013;35(12):1002-1008. doi:10.3109/0142159X.2013.802296
- Kelm Z, Womer J, Walter JK, Feudtner C. Interventions to cultivate physician empathy: a systematic review. BMC Med Educ. 2014;14(1):219. doi:10.1186/1472-6920-14-219
- Mistiaen P, van Osch M, van Vliet L, et al. The effect of patient-practitioner communication on pain: a systematic review. Eur J Pain. 2016;20(5):675-688. doi:10.1002/ejp.797
- Hannawa AF, Shigemoto Y, Little TD. Medical errors: disclosure styles, interpersonal forgiveness, and outcomes. Soc Sci Med. 2016;156:29-38. doi:10.1016/j.socscimed.2016.03.026
- Thirioux B, Birault F, Jaafari N. Empathy is a protective factor of burnout in physicians: new neuro-phenomenological hypotheses regarding empathy and sympathy in care relationship. Front Psychol. 2016;7:763. doi:10.3389/fpsyg.2016.00763
- Wilkinson H, Whittington R, Perry L, Eames C. Examining the relationship between burnout and empathy in healthcare professionals: A systematic review. Burn Res. 2017;6:18-29. doi:10.1016/j.burn.2017.06.003
- Thomas MR, Dyrbye LN, Huntington JL, et al. How do distress and well-being relate to medical student empathy? A multicenter study. J Gen Intern Med. 2007;22(2):177-183. doi:10.1007/s11606-006-0039-6
- Bernardo MO, Cecilio-Fernandes D, Lima ARA, et al. Investigating the relation between self-assessment and patients’ assessments of physicians-in-training empathy: a multicentric, observational, cross-sectional study in three teaching hospitals in Brazil. BMJ Open. 2019;9(6):e029356. doi:10.1136/bmjopen-2019-029356
- Neumann M, Bensing J, Wirtz M, et al. The impact of financial incentives on physician empathy: a study from the perspective of patients with private and statutory health insurance. Patient Educ Couns. 2011;84(2):208-216. doi:10.1016/j.pec.2010.07.012
- Kane GC, Gotto JL, Mangione S, West S, Hojat M. Jefferson Scale of Patient’s Perceptions of Physician Empathy: preliminary psychometric data. Croat Med J. 2007;48(1):81-86. http://www.ncbi.nlm.nih.gov/pubmed/17309143
- Hojat M, DeSantis J, Gonnella JS. Patient perceptions of clinician’s empathy: measurement and psychometrics. J Patient Exp. 2017;4(2):78-83. doi:10.1177/2374373517699273
- Borracci RA, Doval HC, Celano L, Ciancio A, Manente D, Calderón JGE. Patients’ perceptions of argentine physicians’ empathy based on the jefferson scale of patient’s perceptions of physician empathy: psychometric data and demographic differences. Educ Health (Abingdon). 2017;30(1):19-25. doi:10.4103/1357-6283.210513
- Haensch G. Español de América y español de Europa (2a parte). panace@. 2002;3(7):37-64. https://www.tremedica.org/wp-content/uploads/n7_G_Haensch7.pdf
- Haensch G. Español de América y español de Europa (1a parte). panace@. 2001;2(6):63-72. https://www.tremedica.org/wp-content/uploads/n6_G_Haensch.pdf
- Ferreira-Valente A, Costa P, Elorduy M, Virumbrales M, Costa MJ, Palés J. Psychometric properties of the Spanish version of the Jefferson Scale of Empathy: making sense of the total score through a second order confirmatory factor analysis. BMC Med Educ. 2016;16(1):242. doi:10.1186/s12909-016-0763-5
- Alcorta-Garza A, San-Martín M, Delgado-Bolton R, Soler-González J, Roig H, Vivanco L. Cross-validation of the Spanish HP-Version of the Jefferson Scale of Empathy confirmed with some cross-cultural differences. Front Psychol. 2016;7:1002. doi:10.3389/fpsyg.2016.01002
- Delgado-Bolton R, San-Martín M, Alcorta-Garza A, Vivanco L. Empatía médica en médicos que realizan el programa de formación médica especializada. Estudio comparativo intercultural en España. Aten Primaria. 2016;48(9):565-571. doi:10.1016/j.aprim.2015.10.005
- Hojat M, Louis DZ, Maxwell K, Markham F, Wender R, Gonnella JS. Patient perceptions of physician empathy, satisfaction with physician, interpersonal trust, and compliance. Int J Med Educ. 2010;1:83-87. doi:10.5116/ijme.4d00.b701
- García Del Barrio L, Rodríguez-Díez C, Martín-Lanas R, Costa P, Costa MJ, Díez N. Reliability and validity of the Spanish (Spain) version of the consultation and relational empathy measure in primary care. Fam Pract. 2021;38(3):353-359. doi:10.1093/fampra/cmaa135
- Taherdoost H. Validity and reliability of the research instrument; how to test the validation of a questionnaire/survey in a research. International Journal of Academic Research in Management. 2016;5(3):28-36. doi:10.2139/ssrn.3205040
- Terwee CB, Bot SDM, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34-42. doi:10.1016/j.jclinepi.2006.03.012
- Coveney J. Calculated alpha after polichoric factor analysis. Accessed April 5, 2020. http://www.stata.com/statalist/archive/2012-02/msg00696.html
- Zumbo BD, Gadermann AM, Zeisser C. Ordinal versions of coefficients alpha and theta for Likert rating scales. J Mod Appl Stat Methods. 2007;6(1):21-29. doi:10.22237/jmasm/1177992180
- Streiner D, Norman G, Cairney J. Health Measurement Scales: A practical Guide to Their Development and Use. 5th ed. Oxford: Oxford University Press; 2015.
- Kaiser H. An index of factorial simplicity. Psychometrika. 1974;39(1):31-36. doi:10.1007/BF02291575
- Bernardo MO, Cecílio-Fernandes D, Costa P, Quince TA, Costa MJ, Carvalho-Filho MA. Physicians’ self-assessed empathy levels do not correlate with patients’ assessments. Arrieta A, ed. PLOS ONE. 2018;13(5):e0198488. doi:10.1371/journal.pone.0198488
- Katsari V, Tyritidou A, Domeyer PR, Giorgi G. Physicians’ Self-assessed empathy and patients’ perceptions of physicians’ empathy: validation of the Greek Jefferson Scale of Patient Perception of Physician Empathy. BioMed Res Int. 2020;2020:9379756. doi:10.1155/2020/9379756
- Flora DB, Curran PJ. An empirical evaluation of alternative methods of estimation for confirmatory factor analysis with ordinal data. Psychol Methods. 2004;9(4):466-491. doi:10.1037/1082-989X.9.4.466
- Schreiber JB, Nora A, Stage FK, Barlow EA, King J. Reporting structural equation modeling and confirmatory factor analysis results: a review. J Educ Res. 2006;99(6):323-338. doi:10.3200/JOER.99.6.323-338
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6(1):1-55. doi:10.1080/10705519909540118
- Martínez González M, Sánchez Villegas A, Toledo Atucha E, Faulin Fajardo J. Bioestadística Amigable. 3rd ed, Elsevier. Elsevier; 2014.
- Kline JA, Lin MP, Hall CL, et al. Perception of physician empathy varies with educational level and gender of patients undergoing low-yield computerized tomographic imaging. J Patient Exp. 2020;7(3):386-394. doi:10.1177/2374373519838529
- Byrd J, Knowles H, Moore S, et al. Synergistic effects of emergency physician empathy and burnout on patient satisfaction: a prospective observational study. Emerg Med J. 2021;38(4):290-296. doi:10.1136/emermed-2019-209393
- Mohammadi A, Kamali K. Inpatients’ perceptions of physicians’ empathy and their level of satisfaction regarding medical care measured by Jefferson Scale of Patient’s Perceptions of Physician Empathy. J Iran Med Counc. 2019;2(5):120-127.
- Alzayer ZM, Abdulkader RS, Jeyashree K, Alselihem A. Patient-rated physicians’ empathy and its determinants in Riyadh, Saudi Arabia. J Family Community Med. 2019;26(3):199-205. doi:10.4103/jfcm.JFCM_66_19
- Fung CSC, Hua A, Tam L, Mercer SW. Reliability and validity of the Chinese version of the CARE Measure in a primary care setting in Hong Kong. Fam Pract. 2009;26(5):398-406. doi:10.1093/fampra/cmp044
- Mercer SW, Fung CSC, Chan FWK, Wong FYY, Wong SYS, Murphy D. The Chinese-version of the CARE measure reliably differentiates between doctors in primary care: a cross-sectional study in Hong Kong. BMC Fam Pract. 2011;12(1):43. doi:10.1186/1471-2296-12-43
- Aomatsu M, Abe H, Abe K, et al. Validity and reliability of the Japanese version of the CARE measure in a general medicine outpatient setting. Fam Pract. 2014;31(1):118-126. doi:10.1093/fampra/cmt053
- Valls Martínez MC, Ramírez-Orellana A; Valls Martínez M del C. Ramírez-Orellana A. Patient satisfaction in the Spanish National Health Service: partial least squares structural equation modeling. Int J Environ Res Public Health. 2019;16(24):4886. doi:10.3390/ijerph16244886
- Gonzalez AI, Kortlever JTP, Rijk L, Ring D, Brown LE, Reichel LM. Is there a correlation between the patient-doctor relationship questionnaire and other patient-reported experience measures? Patient Exp J. 2020;7(1):44-50. doi:10.35680/2372-0247.1399
- Keulen MHF, Teunis T, Kortlever JTP, Vagner GA, Ring D, Reichel LM. Measurement of perceived physician empathy in orthopedic patients. J Patient Exp. 2020;7(4):600-606. doi:10.1177/2374373519875842
- Domingues AC, Santiago LM, Rodrigues AR, Pires B, Velho D, Ferreira PL. Cross-cultural adaptation and validation of the jefferson scale of patient’s perceptions of physician empathy (JSPPPE) for the portuguese population. Patient Prefer Adherence. 2019;13:1145-1152. doi:10.2147/PPA.S211764
- Kortlever JTP, Ottenhoff JSE, Vagner GA, Ring D, Reichel LM. Visit duration does not correlate with perceived physician empathy. J Bone Joint Surg Am. 2019;101(4):296-301. doi:10.2106/JBJS.18.00372





There are no comments for this article.