Background and Objectives: Training models in the Length of Training Pilot (LOTP) vary. How innovations in training length affect patient visits and resident perceptions of continuity is unknown.
Methods: We analyzed resident in-person patient encounters (2013-2014 through 2018-2019) for each postgraduate year (PGY) and total visits at graduation derived from the Accreditation Council for Graduate Medical Education reports for each LOTP program. We collected data on residents’ perceptions of continuity from annual surveys (2015-2019). We analyzed continuous variables using independent samples t tests with unequal variance and categorical variables using χ2 tests in comparing 3-year (3YR) versus 4-year (4YR) programs.
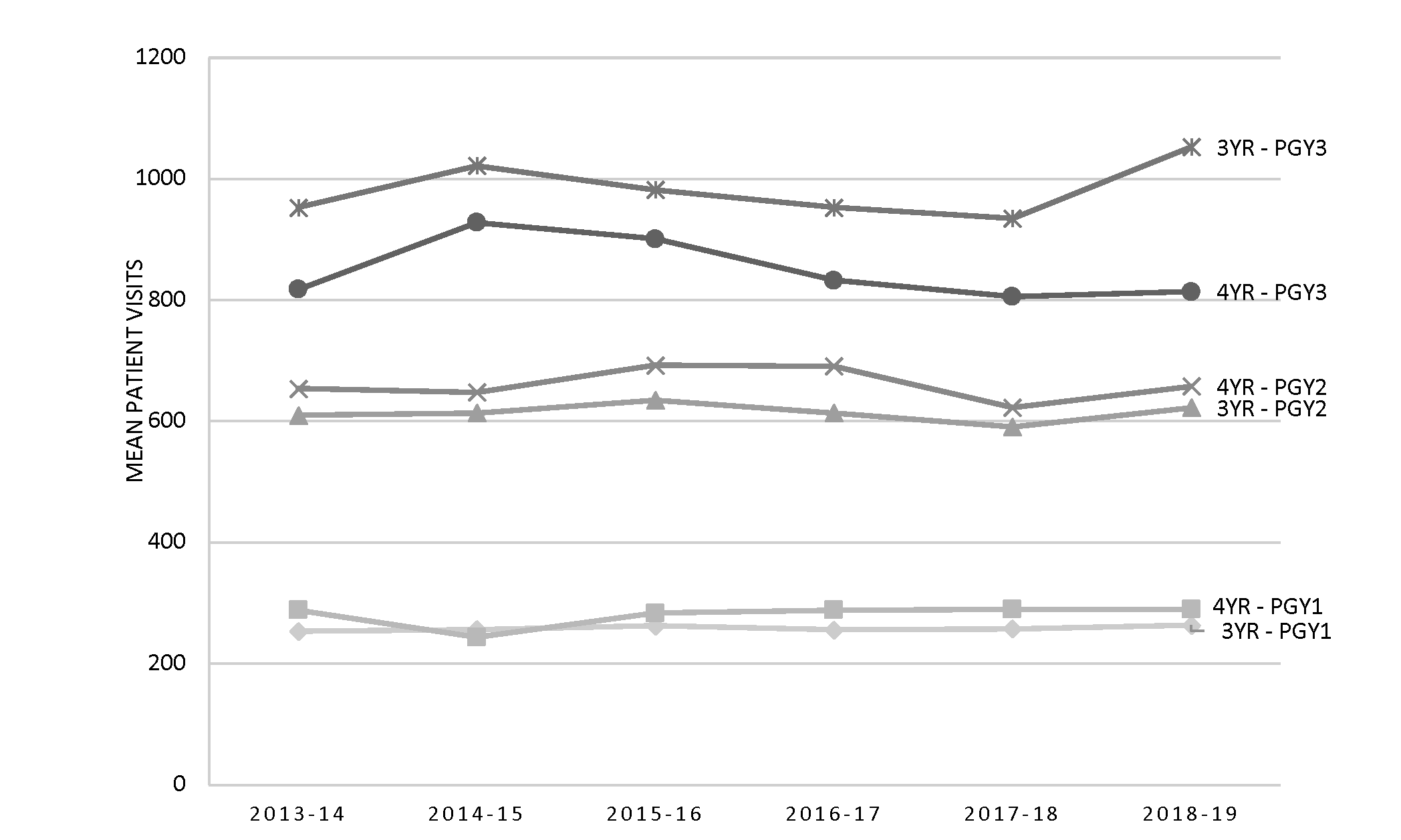
Results: PGY-1 and PGY-2 residents in 4YR programs saw statistically more patients than their counterparts in 3YR programs. In PGY3, 3YR program residents had statistically higher visit volume compared to 4YR program residents. Visits conducted in PGY4 ranged from 832 to 884. The additional year of training resulted in approximately 1,000 more total patient visits. Most residents in 3YR and 4YR programs rated their continuity clinic experience as somewhat or very adequate (range 86.3% to 93.7%), which did not statistically differ according to length of training.
Conclusions: Resident visits were significantly different at each PGY level when comparing 3YR and 4YR programs in the LOTP and the additional year of training resulted in about 1,000 more total visits. Resident perspectives on the adequacy of their continuity clinic experience appeared to not be affected by length of training. Future research should explore how the volume of patient visits performed in residency affects scope of practice and clinical preparedness.
Continuity of care is a foundational aspect of primary care, with many studies indicating it improves patient satisfaction while others indicate it reduces care utilization.1-4 Delivery of care for a defined panel of patients is a cornerstone of family medicine residency training and accounts for the majority of a practicing family physician’s professional time. The training environment can have a lasting effect on the care physicians deliver,5 and patient volume represents an important element of residency training.
The Accreditation Council for Graduate Medical Education (ACGME) requires primary care residencies to create long-term relationships between residents and a panel of patients.6-8 Current family medicine ACGME requirements state residents must be primarily responsible for a panel of continuity patients and provide care for a minimum of 1,650 in-person patient encounters in a family medicine practice site.6 New proposed requirements emphasize the importance of panels even more.9 Resident duty-hour restrictions, electronic health record implementation, and changing residency rotation or program requirements have all been implicated in decreasing resident visit productivity.10, 11
Innovations in graduate medical education (GME) designed to enhance quality continuity experiences for residents include changes in clinic structure,12, 13 curricular changes (Clinic First) that optimize outpatient and inpatient schedules,14-16 and adopting a strong continuity culture.17 Extending family medicine residency training to 4 years might be expected to increase the number of patient visits a resident completes by graduation, which could affect residents’ continuity experiences.
Most studies on the effects of continuity of care report on its influence on the patient experience, quality of care, and cost rather than its effect on providers or trainees. In a qualitative study of how interpersonal continuity of care affects family physicians, experienced physicians describe long-term relationships as a core value in their practices and were important in building trust with patients.18 In this same study, family medicine resident views of relationship continuity were based on their personal health care, and they often learned about continuity of care through role models and theoretical teaching.19 Their views of continuity focused on improved efficiency and confidence.16 In a national cross-sectional study of pediatric residents, residents perceived they had greater continuity with patients and autonomy as they become more senior but lacked involvement in key patient responsibilities across training years.20 We found no studies on family medicine residents’ views of their continuity experience across training years.
The Length of Training Pilot (LOTP) is designed to explore the impact that length of training (3 versus 4 years) has on several outcomes addressed through core research questions.21, 22 While one of our original core questions included studying the effect of length of training on patient continuity, our prior work on measuring continuity revealed inaccuracies in classifying continuity visits in LOTP data.23 We subsequently revised this core LOTP research question to study resident perceptions of continuity. The training models in the LOTP 4-year (4YR) programs are varied; for example, some 4YR programs have a required fourth year with an integrated curriculum and some have an optional fourth year where residents can focus on a specific area of clinical concentration. It is unclear how these different innovations may affect patient visits with residents in each year of training as well as visit totals at graduation. Here, we use data from the LOTP to report on findings that explore the question: What effect does length of training have on patient visits and residents’ perceptions of continuity?
Length of Training Pilot (LOTP)
The LOTP, which runs from 2013 to 2023, is a mixed-methods, prospective case-control pilot study designed to assess how the length of family medicine residency training affects both learner and program outcomes.22 Residencies that wanted to move to a 4YR model or had already transitioned to 4 years of training were selected for the pilot and subsequently matched to 3-year programs (3YR) based on size, geographic region, and clinic setting. Seven 3YR civilian programs, six 4YR civilian programs, and four Navy programs enrolled in the study. We excluded the Navy programs from these analyses because their training structures are different from civilian programs and continuity of care could be affected by military-specific features. Four of the six 4YR programs required 4 years of training for all residents, while two offered an optional fourth year of training where residents typically selected the 4-year option in their second year. To achieve equivalent numbers of residents in 3YR and 4YR groups, two 3YR programs were matched to one 4YR program due to its large size.
The study is overseen by a team of educational researchers at Oregon Health & Science University (OHSU). All LOTP programs obtained Institutional Review Board (IRB) approval and the evaluation team was granted an educational exemption from OHSU’s IRB for study activities (IRB # 9770).
Data Collection
We derived resident visits (in-person encounters) for academic years 2013-2014 through 2018-2019 from the ACGME Family Medicine Specialty Data Reports for each program as well as the national reports for all US programs.24 Programs downloaded their annual reports and sent them to the OHSU evaluation team. The aggregated patient visit data on the reports (mean, median, standard deviation) for each postgraduate year (PGY) and the total visits at graduation were recorded in our database. We compared total visits for residents in 4YR required programs and 4YR optional programs to the same variables for residents in their matched 3YR comparator programs. Because data were normally distributed, we report means and standard deviations in our final comparisons between groups.
We collected characteristics of residents and their attitudes about continuity of care using a resident survey administered annually to all residents in the LOTP. Although the LOTP began in 2013, questions on continuity of care were added to the resident survey in 2015 after discovering the challenges associated with collecting actual continuity visit data (eg, variability in empanelment approaches and difficulty in attaining continuity counts for individual residents). We used only the most recent survey of each resident enrolled in an LOTP program to analyze their characteristics and used all annual surveys completed between 2015 and 2020 for the analysis of attitudes. Residents were asked:
Considering your interpersonal continuity with patients (defined as an ongoing clinician-patient relationship characterized by loyalty and trust), do you think your work in your continuity clinic provides (adequacy rating) continuity of care with patients in my panel?
The rating scale used 1: extremely inadequate; 2: somewhat inadequate; 3: neutral–neither adequate nor inadequate; 4: somewhat adequate; and 5: very adequate. Residents also rated their agreement with statements about how continuity of care with patients in their panel affects them. Response rates for the resident survey ranged from 96.1% to 97.3%.
Statistical Analyses
We used descriptive statistics to characterize residents’ demographic information by length of training group. We analyzed continuous variables comparing the two groups (3YR versus 4YR) using independent samples t tests with unequal variance and categorical variables were assessed using χ2 tests.
To compare the number of patient visits per resident based on length of training, we used two analytic approaches. First, we used mean and standard deviations to summarize the number of patient visits across years (2013-2014 to 2018-2019) at each PGY level according to length of training. Second, we stratified the total number of patient visits at graduation across years (2015-2016 to 2018-2019) according to length of training for programs that required 4YRs or had an optional 4 YR and we then compared them to their matched 3YR programs. In both approaches, we derived the reported P values from independent sample t tests assessing the overall mean differences according to length of training.
We used resident surveys to study differences between 3YR and 4YR residents for each of the two perceptions (continuity-of-clinic experience and continuity-of-care effects). We collapsed the original five item Likert scale for the continuity of clinic experience questions to three categories (1=extremely or somewhat inadequate; 2=neutral; and 3=somewhat or very adequate) according to resident’s PGY and program length. We collapsed the original five-item Likert scale for the four continuity of care effects variables to three categories (1=strongly or somewhat disagree; 2=neutral; and 3=somewhat or strongly agree) according to program length. We employed χ2 and Fisher’s exact test of homogeneity to examine whether differences in proportion distribution of item responses according to program length existed for both continuity of clinic experience and of care effects, respectively.
Notably, while some summary tables were presented showing study year, year played no role in the two-sample t tests, given the hypothesis tested involved comparing the overall mean number of patients visit according to length of training. We performed analyses using R software version 4.1.1.25 All statistical tests were two-sided, and we set α at 0.05 to determine statistical significance.
Residents in both study groups were predominantly female, non-Hispanic White, married or partnered, not parents, and US medical school graduates. These characteristics were not statistically different among residents training in 3YR versus 4YR programs (Table 1 ). Compared to national data, LOTP residents were more likely to be slightly younger, female, White, and have graduated from a US medical school.
|
Characteristic
|
3YR Residents
|
4YR Residents
|
National
Data
b
|
3YR vs 4YR Comparison
|
|
n=471
|
n=513
|
n=14416
|
P
Value
c
|
|
Mean Age in Years (SD)
|
30.9 (4.0)
|
30.9 (3.4)
|
32.4
|
.875
|
|
Gender Identity
|
n (%)
|
n (%)
|
%
|
|
|
Male
|
167 (35.5%)
|
207 (40.4%)
|
45.9
|
.419
|
|
Female
|
302 (64.1%)
|
303 (59.1%)
|
54.1
|
|
Nonbinary
|
1 (0.2%)
|
1 (0.2%)
|
|
|
Missing
|
1 (0.2%)
|
2 (0.4%)
|
|
|
Race/Ethnicity
|
|
Non-Hispanic White
|
290 (61.6%)
|
347 (67.6%)
|
55.8
|
.309
|
|
Hispanic
|
45 (9.6%)
|
38 (7.4%)
|
7.1
|
|
Non-Hispanic Black
|
21 (4.5%)
|
12 (2.3%)
|
7.2
|
|
Non-Hispanic Asian or PI
|
85 (18.0%)
|
83 (16.2%)
|
22.8
|
|
Non-Hispanic AI/AN
|
1 (0.2%)
|
2 (0.4%)
|
0.5
|
|
Non-Hispanic other
|
9 (1.9%)
|
10 (1.9%)
|
6.6
|
|
Multiracial
|
14 (3.0%)
|
18 (3.5%)
|
|
|
Missing
|
6 (1.3%)
|
3 (0.6%)
|
1.4
|
|
Marital Status
|
|
Single
|
220 (46.7%)
|
220 (42.9%)
|
|
.237
|
|
Married/Partnered
|
239 (50.7%)
|
284 (55.4%)
|
|
|
Separated
|
2 (0.4%)
|
2 (0.4%)
|
|
|
Divorced
|
8 (1.7%)
|
5 (1.0%)
|
|
|
Widowed
|
0 (0.0%)
|
2 (0.4%)
|
|
|
Missing
|
2 (0.4%)
|
0 (0.0%)
|
|
|
Parental Status (Have Children)
|
|
No
|
367 (77.9%)
|
380 (74.1%)
|
|
.366
|
|
Yes
|
99 (21.0%)
|
126 (24.6%)
|
|
|
Missing
|
5 (1.1%)
|
7 (1.4%)
|
|
|
US Medical School Graduate
|
|
|
|
|
Yes
|
407 (86.4%)
|
449 (87.5%)
|
69.1
|
.442
|
|
No
|
62 (13.2%)
|
59 (11.5%)
|
30.9
|
|
Missing
|
2 (0.4%)
|
5 (1.0%)
|
|
Patient Visits
The mean number of visits in the first 3 years of training were statistically different between the study groups (Table 2 and Figure 1). PGY1 residents in 4YR programs saw more patients than their counterparts in 3YR programs (overall mean 4YR=282, 3YR=257; P=.007). PGY-2 residents in 4YR programs saw more patients than their counterparts in 3YR programs (overall mean 4YR=666, 3YR=608; P<.001). This difference was reversed at the PGY-3 level with 3YR program residents having higher patient visit volume compared to 4YR program residents (overall mean 4YR=864, 3YR=975; P<.001). In study years with complete data from the four required 4YR programs, visits conducted at the PGY-4 level ranged from 832 to 884.
|
|
|
|
LOTP Study Years
|
|
|
|
|
PGY Level
|
Program Length
|
2013-14
|
2014-15
|
2015-16
|
2016-17
|
2017-18
|
2018-19
|
Overall Mean (SD)
|
P
Value
a
(3YR vs 4YR)
|
|
Program Level Visits Mean (SD)
|
PGY1
|
3
|
254 (74)
|
257 (69)
|
263 (59)
|
256 (59)
|
258 (56)
|
264 (66)
|
257 (62)
|
.007
|
|
4
|
289 (53)
|
286 (61)
|
284 (61)
|
289 (46)
|
290 (43)
|
290 (39)
|
282 (60)
|
|
|
Nationalc
|
238 (80)
|
242 (81)
|
247 (87)
|
247 (87)
|
248 (88)
|
249 (89)
|
|
|
|
PGY2
|
3
|
610 (71)
|
614 (80)
|
635 (60)
|
614 (60)
|
591 (84)
|
623 (101)
|
608 (75)
|
0.001
|
|
4
|
654 (77)
|
648 (86)
|
693 (94)
|
691 (70)
|
623 (93)
|
658 (73)
|
666 (86)
|
|
|
National
|
612 (140)
|
622 (136)
|
623 (140)
|
616 (133)
|
607 (139)
|
605 (140)
|
|
|
|
PGY3
|
3
|
953 (136)
|
1,022 (140)
|
982 (108)
|
953 (140)
|
935 (106)
|
1,053 (223)
|
975 (138)
|
<.001
|
|
4
|
818 (105)
|
928 (112)
|
901 (90)
|
833 (70)
|
806 (119)
|
814 (126)
|
864 (119)
|
|
|
National
|
937 (181)
|
945 (172)
|
948 (164)
|
926 (159)
|
924 (165)
|
928 (162)
|
|
|
|
PGY 4
b
|
3
|
NA
|
NA
|
NA
|
NA
|
NA
|
NA
|
NA
|
NA
|
|
4
|
941 (16)
|
581 (450)
|
691 (365)
|
884 (228)
|
848 (156)
|
832 (227)
|
|
809 (239)
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Total Visits at Graduation
Mean (SD)
|
Programs
|
|
|
|
|
|
|
|
|
|
3YR Comparators (n=4)
|
NA
|
NA
|
1,800 (139)
|
1,758 (64)
|
1,736 (66)
|
1754 (88)
|
1,757 (75)
|
<.001
|
|
4YR Required
d
(n=4)
|
NA
|
NA
|
2,306 (774)
|
2,893 (181)
|
2,770 (117)
|
2691 (153)
|
2,716 (314)
|
|
Difference between means
|
|
|
506
|
1,135
|
1034
|
937
|
|
|
|
|
|
|
|
|
|
|
|
|
|
3YR Comparators (n=3)
|
NA
|
NA
|
1,991 (238)
|
2,001 (288)
|
1,916 (260)
|
1,961 (241)
|
1,967 (222)
|
.874
|
|
4YR Optional (n=4)
e
|
NA
|
NA
|
1,847 (15)
|
1,903 (148)
|
2,105 (356)
|
2,080 (296)
|
1,984 (219)
|
|
National (all residencies)
|
|
|
1,823 (204)
|
1,821 (208)
|
1,814 (203)
|
1,808 (187)
|
|
|
Mean visits at the PGY-1 level for both 3YR and 4YR programs exceeded the national mean for all family medicine programs for all study years. At the PGY-2 level, the 4YR program mean visits exceeded the national mean for all study years whereas the 3YR programs were comparable to the national mean for all study years. At the PGY-3 level, the 3YR program mean visits exceeded the national mean for all study years whereas the 4YR programs were below the national mean for all study years.
With an additional year of training, residents in required 4YR programs completed a significantly higher number of visits at graduation (Table 2 ). Based on the 3 study years with complete data for all PGY levels in required 4YR programs, residents completed approximately 1,000 more visits at graduation. Total visits at graduation were not significantly different between residents in optional 4YR programs compared to their 3YR program counterparts. Visit totals in 4YR optional programs include residents who completed their training in 3 years in addition to those completing 4 years of training.
Resident Attitudes About Continuity of Care
Most residents at all PGY levels in both 3YR and 4YR programs rated how well their work in their clinic provided continuity of care with their patients as somewhat or very adequate (range 86.3% to 93.7%), which did not statistically differ according to length of training (P values>.67;
Table 3
).
|
|
Program Length
|
No. of Residents
|
Extremely or Somewhat Inadequate
|
Neutral – Neither Adequate nor Inadequate
|
Somewhat or Very Adequate
|
P Value
b
|
|
PGY1
|
3
|
288
|
11 (3.8%)
|
27 (9.4%)
|
250 (86.8%)
|
.973
|
|
4
|
313
|
13 (4.2%)
|
30 (9.6%)
|
270 (86.3%)
|
|
PGY2
|
3
|
276
|
16 (5.8%)
|
16 (5.8%)
|
244 (88.4%)
|
.872
|
|
4
|
308
|
15 (4.9%)
|
19 (6.2%)
|
274 (89.0%)
|
|
PGY3
|
3
|
285
|
7 (2.5%)
|
11 (3.9%)
|
267 (93.7%)
|
.670
|
|
4
|
295
|
7 (2.4%)
|
16 (5.4%)
|
272 (92.2%)
|
|
PGY4
|
3
|
NA
|
NA
|
NA
|
NA
|
NA
|
|
4
|
184
|
6 (3.3%)
|
6 (3.3%)
|
172 (93.5%)
|
Residents from both 3YR and 4YR programs had similar views of how continuity of care affected their work and their views were not statistically different except for communication effectiveness with patients (P=.018;
Table 4). Residents in both study groups agreed or strongly agreed that continuity of care with patients in their panel helped them better understand patient needs (3YR=98%, 4YR=98.3%). Similarly, high percentages of residents in both 3YR and 4YR programs agreed or strongly agreed that continuity of care with patients helped them have a greater impact on health outcomes and improved resident job satisfaction.
|
Continuity of Care With Patients in My Panel:
|
Program Length
|
No. of Resident Surveys
|
Strongly/Somewhat Disagree
|
Neutral
|
Somewhat/Strongly Agree
|
P
Value
b
|
|
Helps me communicate more effectively with patients
|
3
|
853
|
5 (0.6%)
|
12 (1.4%)
|
836 (98.0%)
|
.018
|
|
4
|
1102
|
0 (0%)
|
22 (2.0%)
|
1080 (98.0%)
|
|
Helps me better understand specific patient needs
|
3
|
855
|
2 (0.2%)
|
15 (1.8%)
|
838 (98.0%)
|
.739
|
|
4
|
1102
|
1 (0.1%)
|
18 (1.6%)
|
1083 (98.3%)
|
|
Helps me have a greater impact on patient health outcomes
|
3
|
855
|
2 (0.2%)
|
24 (2.8%)
|
829 (97.0%)
|
.640
|
|
4
|
1102
|
1 (0.1%)
|
27 (2.5%)
|
1074 (97.4%)
|
|
Improves my job satisfaction
|
3
|
854
|
4 (0.5%)
|
40 (4.7%)
|
810 (94.8%)
|
.223
|
|
4
|
1099
|
9 (0.8%)
|
37 (3.4%)
|
1053 (95.8%)
|
Our study presents the resident visit productivity and views of their continuity experience across training years in the LOTP programs. When comparing visits in each year of training in 3YR versus 4YR programs, we found significant differences in the mean number of visits performed by residents with higher volumes in the first 2 years of residency in 4YR programs and lower volumes at the PGY3 level in 4YR programs. This may be due to the 4YR programs having an additional year to spread out the number of clinic sessions resulting in a lower volume in the third year. Additionally, the 4YR programs expanded their curricula so residents in these programs were exposed to additional training experiences that may have affected their clinic sessions/visit volume especially in the PGY3 and PGY4 years. The number of total visits completed at graduation has consistently been around 1,800 visits in all family medicine programs for the past several years24 and resident visit productivity in the LOTP programs was similar to national data.
The additional year of training in the programs with a required 4-year model resulted in approximately 1,000 more patient visits. Time in clinic and panel size have an impact on resident continuity with patients.26 Our findings provide an estimate of the additional resident productivity that may occur if training is extended to 4 years, which could counterbalance restricting forces such as duty-hour restrictions or competing rotation requirements. Given that total visits is a limited measure of clinic productivity, in future studies of the impact of extending the length of residency training additional measures of clinic efficiency, clinical preparedness and quality of care should be explored.
Along with the additional clinical experience residents gain with a higher patient volume, the additional visits can be a source of revenue for residencies. Financing an additional year of training is one barrier to implementing a 4-year training model. The required 4YR programs have demonstrated sustainable funding models and the increased clinical revenue generated by fourth year residents is a viable way to finance the additional year of training. 27, 28
Fundamental to family medicine residency training is the continuity clinic experience, which provides residents with the opportunity to forge continuous relationships with patients. In this study of resident perceptions of their continuity clinic experience, a high percentage of residents rated that working in their clinic was somewhat or very adequate in providing continuity of care with patients in their panel. This was the case regardless of length of training. Notably, the proportion distribution of resident responses about the adequacy of continuity of care across all study years and between PGY levels showed no significant differences.
The vast majority of residents in both study groups agreed that continuity of care with patients in their panel helped them communicate more effectively with patients and better understand their needs. This is similar to another study showing that residents perceived that relationship continuity led to improved efficiency and confidence.19 LOTP residents also viewed continuity of care with patients as improving job satisfaction and helping them have a greater impact on health outcomes. A systematic review has validated the association between continuity of care and improved quality of care and patient outcomes.4, 8
As the definition of continuity evolves to include continuity with an interprofessional team, the result may be new approaches to studying continuity, as patients ultimately may feel a tighter connection to other care team members compared with residents. Similarly, contacts with other members of the team will need to be considered in measures of productivity in primary care when delivering patient-centered care. The expansion of virtual visits and telehealth during the COVID-19 pandemic are emerging aspects of productivity that need to be taken into account. These visits may become a more substantial proportion of clinic visits and may affect rates of continuity of care overall.
The new proposed ACGME Program Requirements for Family Medicine slated to go into effect July 1, 2023 have eliminated the requirement of 1,650 visits at graduation while also adding requirements that maximize a resident’s continuity patient panel and engage team-based coverage.9 Telehealth visits are also mentioned in the draft requirements as a part of residents’ patient encounters. These new requirements will likely include measures of continuity with the resident and other team members in more meaningful ways that address patient outcomes. The time is right for family medicine programs to develop new and innovative approaches to promoting a continuity experience for residents.
A study of over 8,000 family physicians seeking initial recertification from 2013 to 2016 showed that individual, practice, and residency characteristics were all associated with scope of practice.28 It is not yet known how the volume of patient visits performed in residency affects the individual’s eventual scope of practice or preparedness for independent clinical practice. Future analyses in the LOTP, conducted once data collection for all study cohorts is completed in 2023, will likely shed light on this question.
The strengths of this study include data capture of a resident survey from more than 95% of residents participating in the LOTP as well as capturing visit data annually from 100% of the programs. Although we weren’t able to conduct a statistical analysis of visits from LOTP programs compared to national visit data for all residencies, having national data provides meaningful benchmarks.
This study has limitations. Generalizability of our findings is limited given the small number of programs enrolled in the LOTP. Converting from 3 to 4 years of training is a significant endeavor, and programs that chose to undertake such an effort may have greater resources or flexibility in affecting resident visit productivity compared to other residencies. We matched 3YR programs to 4YR programs based on geographic location, size, and clinic setting, and our insignificant findings between resident demographics in the study groups suggest our matching strategy was successful. However, since there were a higher number of patient visits in this study for 3YR programs compared to the national mean, they may not have been representative of programs nationally. Another limitation is that we were only analyzing resident visits in total, not the actual number of continuity visits they performed due to wide variation in LOTP programs’ ability to obtain these data and the varying continuity measures used. Thus, we were unable to correlate resident attitudes about continuity with the number of continuity visits performed. Comparison of continuity between programs would likely be improved if standardized measures were used for all family medicine residencies. 16
In-person patient visits performed by residents were significantly different at each PGY level when comparing 3YR and 4YR programs in the LOTP and a fourth year of training resulted in an addition of approximately 1,000 visits per resident at graduation. Resident perspectives on the adequacy of their continuity clinic experience in providing continuity of care with their patients appear to not be affected by length of training. Future research should explore how the volume of patient visits performed in residency affects scope of practice and clinical preparedness.
Financial Support
This research project was approved and directed by the Accreditation Council for Graduate Medical through funding by the American Board of Family Medicine (ABFM) Foundation. Authors included on this article represent the project steering committee that includes representation from the ACGME Review Committee for Family Medicine, American Board of Family Medicine, Association of Family Medicine Residency Directors, and American Academy of Family Physicians.
References
-
Adler R, Vasiliadis A, Bickell N. The relationship between continuity and patient satisfaction: a systematic review. Fam Pract
. 2010;27(2):171-178. doi:10.1093/fampra/cmp099
-
Saultz JW, Lochner J. Interpersonal continuity of care and care outcomes: a critical review. Ann Fam Med
. 2005;3(2):159-166. doi:10.1370/afm.285
-
Bazemore A, Petterson S, Peterson LE, Bruno R, Chung Y, Phillips RL Jr. Higher primary care physician continuity is associated with lower costs and hospitalizations. Ann Fam Med
. 2018;16(6):492-497. doi:10.1370/afm.2308
-
van Walraven C, Oake N, Jennings A, Forster AJ. The association between continuity of care and outcomes: a systematic and critical review. J Eval Clin Pract
. 2010;16(5):947-956. doi:10.1111/j.1365-2753.2009.01235.x
-
Phillips RL Jr, Petterson SM, Bazemore AW, Wingrove P, Puffer JC. The effects of training institution practice costs, quality, and other characteristics on future practice. Ann Fam Med
. 2017;15(2):140-148. doi:10.1370/afm.2044
-
-
-
-
-
Lesko S, Hughes L, Fitch W, Pauwels J. Ten-year trends in family medicine residency productivity and staffing: impact of electronic health records, resident duty hours, and the medical home. Fam Med. 2012;44(2):83-89.
-
Lindbloom EJ, Ringdahl E. Resident duty hour changes: impact in the patient-centered medical home. Fam Med. 2014;46(6):463-466.
-
Neher JO, Kelsberg G, Oliveira D. Improving continuity by increasing clinic frequency in a residency setting. Fam Med. 2001;33(10):751-755.
-
Merenstein D, Damico F, Devine B, et al. Longitudinal versus traditional residencies: a study of continuity of care. Fam Med. 2001;33(10):746-750.
-
Gupta R, Barnes K, Bodenheimer T. Clinic First: 6 actions to transform ambulatory residency training. J Grad Med Educ
. 2016;8(4):500-503. doi:10.4300/JGME-D-15-00398.1
-
Zeller TA, Ewing JA, Asif IM. Prevalence of Clinic First curricula: a survey of AFMRD members. Fam Med
. 2019;51(4):338-343. doi:10.22454/FamMed.2019.666943
-
Paul KJ, Hidaka BH, Ford P, Morris C. Measuring greater patient-provider continuity in a clinic-first family medicine residency curriculum. Perm J
. 2021;25(20):20.290. doi:10.7812/TPP/20.290
-
Dubé K, Gupta R, Kong M, Knox M, Bodenheimer T. Continuity of care in residency teaching practices: lessons from “bright spots. Perm J
. 2018;22(3):18-028. doi:10.7812/TPP/18-028
-
Schultz K, Delva D, Kerr J. Emotional effects of continuity of care on family physicians and the therapeutic relationship. Can Fam Physician. 2012;58(2):178-185.
-
Delva D, Kerr J, Schultz K. Continuity of care: differing conceptions and values. Can Fam Physician. 2011;57(8):915-921.
-
Feigelman S, Olsson J, Drutz J, Dungy CI, Lopreiato J, Serwint JR; Continuity Research Network (CORNET) of the Ambulatory Pediatric Association. Changes in pediatric residents’ perceptions of their continuity experience during their training: a national study. Ambul Pediatr
. 2005;5(4):221-227. doi:10.1367/A04-137R1.1
-
-
Carek PJ. The length of training pilot: does anyone really know what time it takes? Fam Med. 2013;45(3):171-172.
-
Carney PA, Conry CM, Mitchell KB, et al. The importance of and the complexities associated with measuring continuity of care during resident training: possible solutions do exist. Fam Med. 2016;48(4):286-293..
-
-
-
Walker J, Payne B, Clemans-Taylor BL, Snyder ED. Continuity of care in resident outpatient clinics: a scoping review of the literature. J Grad Med Educ
. 2018;10(1):16-25. doi:10.4300/JGME-D-17-00256.1
-
Douglass AB, Barr WB, Skariah JM, et al. Financing the fourth year: experiences of required 4-year family medicine residency programs. Fam Med
. 2021;53(3):195-199. doi:10.22454/FamMed.2021.249809
-
Carney PA, Ericson A, Conry CM, et al. Financial considerations associated with a fourth year of residency training in family medicine: findings from the Length of Training Pilot Study. Fam Med
. 2021;53(4):256-266. doi:10.22454/FamMed.2021.406778



There are no comments for this article.